Pharmacogenomics: How Your Genes Affect Your Medications
When you take a pill, your body doesn’t just process it the same way everyone else does. Pharmacogenomics, the study of how genes influence how your body responds to drugs. Also known as personalized medicine, it’s the reason one person can take a standard dose of a drug and feel fine, while another gets sick from the same pill. This isn’t guesswork—it’s science backed by real data from millions of patients. Your DNA holds clues about how fast you break down medications, whether you’re likely to have side effects, and even if a drug will work at all.
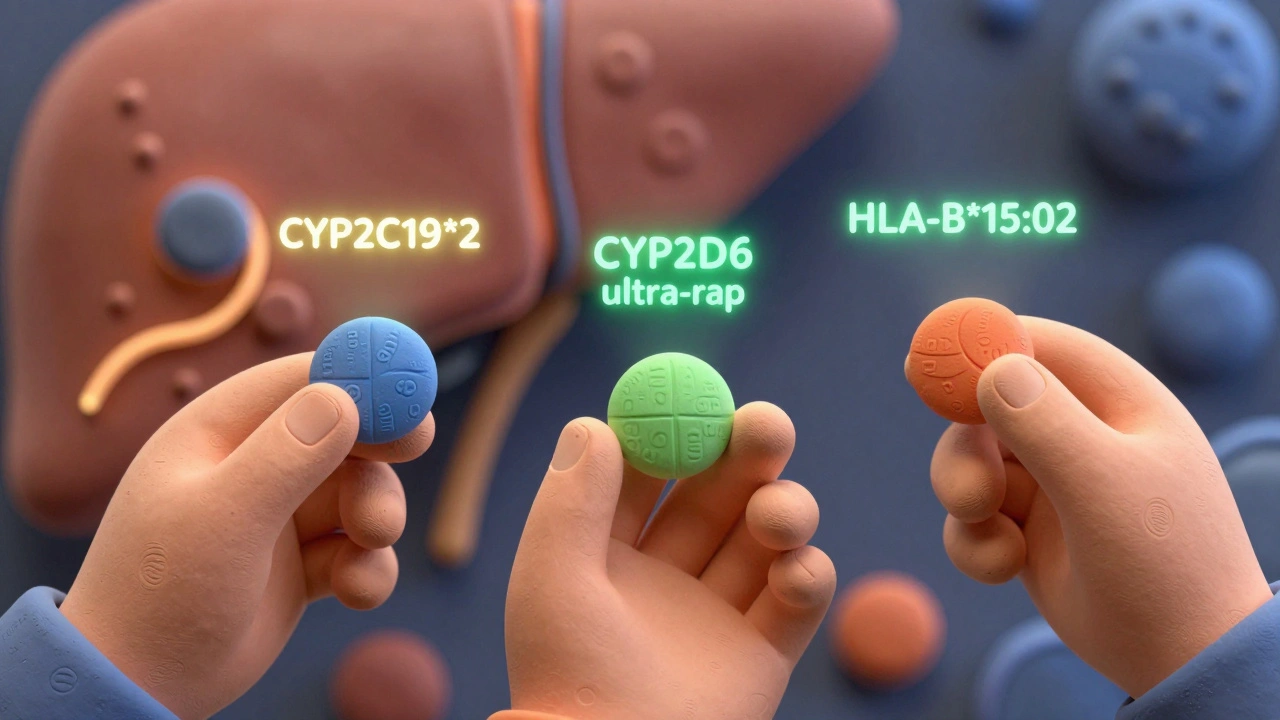
Take drug metabolism, how your liver processes medications using enzymes like CYP2D6 and CYP2C19. Some people have gene variants that make these enzymes work too fast—meaning the drug leaves their system before it can help. Others have slow enzymes, so the drug builds up and causes toxicity. This is why warfarin, antidepressants, and even codeine can be dangerous for some and harmless for others. Medication safety, especially with psychiatric drugs, blood thinners, and cancer treatments, depends heavily on knowing your genetic profile. A simple saliva test can tell your doctor whether you’re a poor, intermediate, normal, or ultra-rapid metabolizer—no more trial and error.
It’s not just about avoiding bad reactions. Pharmacogenomics helps doctors pick the right drug the first time. For example, if you have a certain gene variant, you might respond better to one antidepressant over another, or need half the usual dose of a painkiller. This cuts down on wasted time, unnecessary side effects, and hospital visits. Even something as common as aspirin can be affected—some people’s genes make them resistant to its heart-protective effects. And while this tech is still growing, it’s already changing how cancer drugs like tamoxifen and clopidogrel are prescribed. You don’t need to be a cancer patient to benefit. If you’ve ever been told a medication didn’t work for you—or gave you side effects others didn’t get—pharmacogenomics might explain why.
Below, you’ll find real-world guides on how genes interact with common drugs, how to spot dangerous interactions, and how to talk to your doctor about testing. From QT prolongation risks with antibiotics to how fiber supplements mess with thyroid meds, these posts connect the dots between your biology and your medicine cabinet. This isn’t theory. It’s what’s already happening in clinics and pharmacies—and it’s about to become part of your care too.
Ethnicity and Drug Response: How Genetics Shape Medication Effectiveness
Harrison Greywell Dec, 1 2025 13Ethnicity influences how people respond to medications due to genetic differences in drug metabolism. Learn how CYP enzymes, pharmacogenomics, and ancestry impact drug effectiveness and safety across populations.
More Detail