Macrolides: What They Are, How They Work, and What You Need to Know
When your doctor prescribes an antibiotic for a stubborn sinus infection, strep throat, or even some types of pneumonia, they might reach for a macrolide, a class of antibiotics that stop bacteria from making proteins they need to survive. Also known as protein synthesis inhibitors, macrolides are one of the most commonly used antibiotic families in outpatient care. Unlike penicillin, they’re often chosen when someone has an allergy—or when the infection doesn’t respond to first-line drugs. The big names you’ve probably heard are azithromycin, a once-daily pill often used for chest infections and sexually transmitted infections, clarithromycin, a go-to for H. pylori and sinus infections, and erythromycin, the original macrolide, still used for skin and respiratory bugs.
These drugs don’t kill bacteria outright—they stop them from multiplying. That’s why they’re called bacteriostatic. They work by latching onto the bacterial ribosome, the tiny factory inside the cell that builds proteins. No protein production? The bacteria can’t grow, spread, or cause more damage. Your immune system then cleans up the rest. This mechanism makes macrolides useful against a range of bugs, including some that are resistant to other antibiotics. But they’re not magic. They won’t touch viruses, and overuse leads to resistance. That’s why you’ll see them used more selectively now than in the past.
What’s tricky with macrolides is how they interact with other meds. Azithromycin can mess with heart rhythms if you’re already on certain antiarrhythmics. Clarithromycin slows down how your liver breaks down statins, blood thinners, and even some antidepressants—raising the risk of side effects. And yes, even something as simple as taking them with food can change how well they work. Erythromycin? Best on an empty stomach. Azithromycin? Can go with or without. It’s not one-size-fits-all.
Side effects? Stomach upset is common—nausea, diarrhea, cramps. That’s why some people switch from erythromycin to azithromycin; it’s gentler on the gut. Rare but serious? Liver problems, hearing changes, or an irregular heartbeat. If you’ve ever had a bad reaction to one macrolide, you might react to others too—they’re closely related chemically.
What you’ll find in this collection are real-world guides on how macrolides fit into daily life: how to take them safely, what to avoid mixing them with, how they compare to other antibiotics, and what to do if you experience side effects. You’ll also see how they’re used for conditions like rosacea (topical), how they interact with fiber supplements, and why timing matters when you’re on multiple meds. There’s no fluff—just clear, practical info based on how these drugs are actually prescribed and used today.
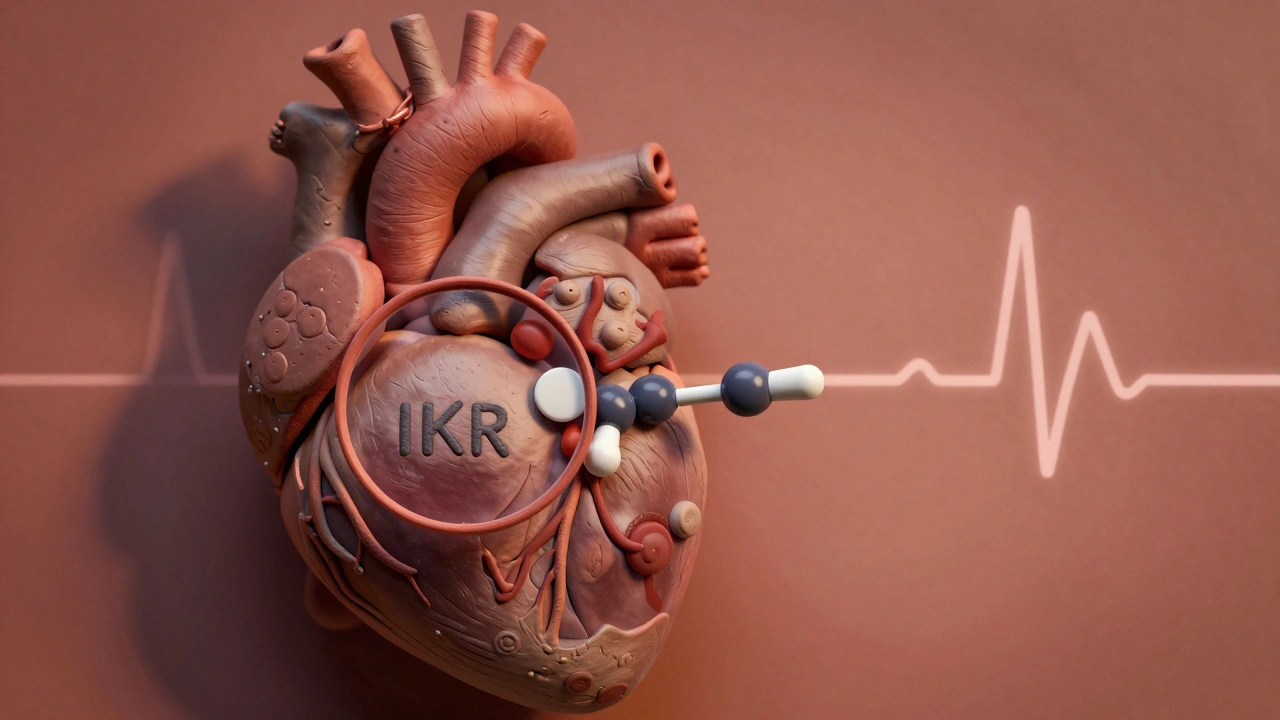
Macrolides and QT-Prolonging Drugs: Understanding the Arrhythmia Risk
Harrison Greywell Dec, 4 2025 8Macrolide antibiotics like azithromycin and clarithromycin can prolong the QT interval and trigger dangerous heart rhythms, especially in older adults or those on multiple medications. Learn who’s at risk and how to stay safe.
More Detail