Aminoglycoside Ototoxicity: How These Antibiotics Cause Permanent Hearing and Balance Damage
Jan, 28 2026
Aminoglycoside Ototoxicity Risk Calculator
This tool estimates your risk of permanent hearing and balance damage from aminoglycoside antibiotics based on key factors discussed in the article. Results are for informational purposes only.
Your Risk Assessment
When you're fighting a life-threatening infection, antibiotics are a lifeline. But some of the most powerful ones - aminoglycosides like gentamicin, amikacin, and tobramycin - come with a hidden cost: aminoglycoside ototoxicity. This isn’t a rare side effect. It’s a predictable, often permanent injury to your hearing and balance system that affects up to half of patients who receive these drugs. And too often, it happens without warning.
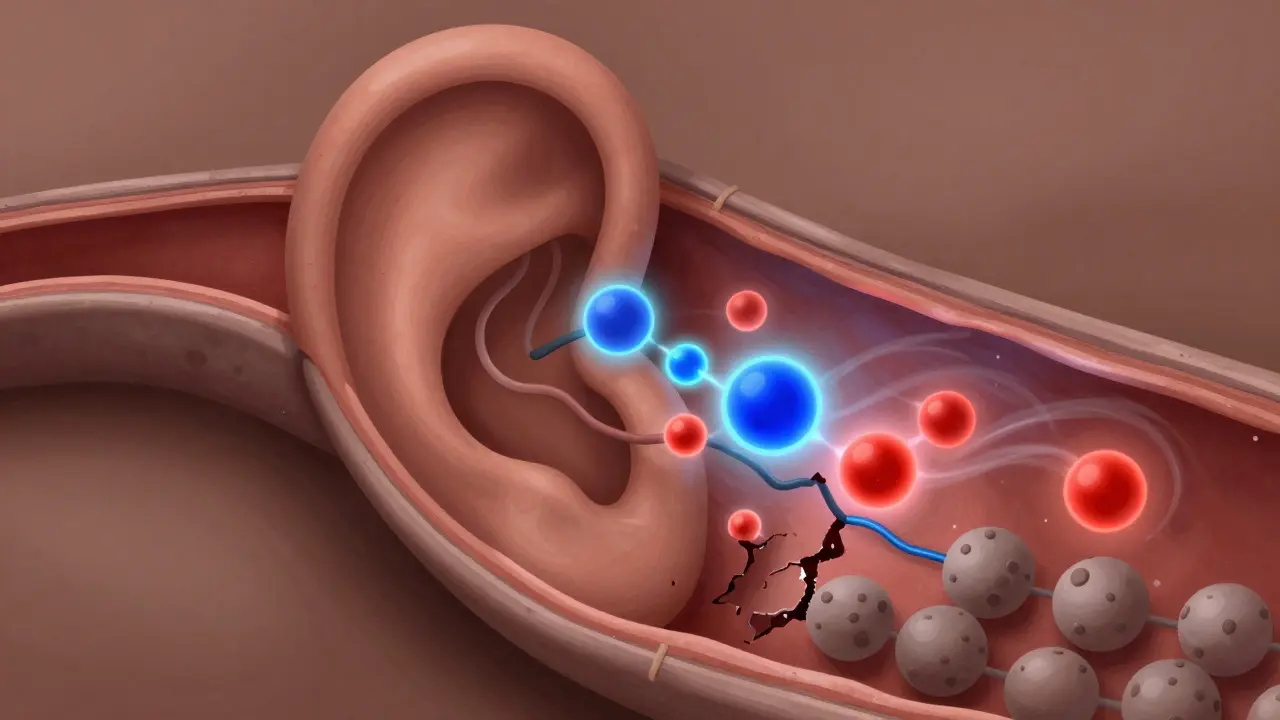
How Aminoglycosides Destroy Inner Ear Cells
Aminoglycosides don’t just kill bacteria. They also slip into the inner ear and start killing your sensory hair cells - the tiny, delicate structures in your cochlea and vestibular system that turn sound and head movement into nerve signals your brain understands. Once these cells die, they don’t grow back. That’s why the damage is permanent. These antibiotics enter the inner ear through the bloodstream, crossing the blood-labyrinth barrier, or sometimes directly through the round window membrane. Once inside, they trigger a chain reaction: they overactivate NMDA receptors, flood cells with nitric oxide, and generate free radicals that shred cellular machinery. The result? Both apoptosis (programmed cell death) and necrosis (cell rupture). Unlike cisplatin, which mostly causes apoptosis, aminoglycosides do both - making their destruction faster and more chaotic. The damage starts in the base of the cochlea, where high-frequency hearing happens. That’s why the first sign isn’t difficulty understanding speech - it’s trouble hearing birds chirping, alarms beeping, or children’s voices. By the time standard hearing tests catch it, the damage is often already done.Vestibular Damage: When Your Balance Disappears
Hearing loss gets most of the attention, but vestibular damage is just as serious - and often overlooked. About 15% to 30% of patients on aminoglycosides develop vestibular toxicity. This isn’t just dizziness. It’s a complete loss of balance control. Patients describe it as walking on a boat, constant motion sickness, or the world tilting when they turn their head. In severe cases, like the 34-year-old patient documented at Johns Hopkins after 10 days of gentamicin, the damage is bilateral and total. Recovery takes months of intensive vestibular rehabilitation - and some never fully regain stability. Unlike hearing loss, which can sometimes be masked by background noise, vestibular damage hits you in everyday moments: stepping off a curb, getting out of bed, walking in the dark. It’s not just inconvenient - it’s dangerous. Falls increase. Confidence drops. Quality of life plummets.Genetics Make Some People Far More Vulnerable
Not everyone who gets aminoglycosides loses their hearing. But some people are walking time bombs - and they don’t even know it. A small group carries a mutation in their mitochondrial DNA - specifically the A1555G or C1494T changes in the 12S rRNA gene. These mutations make their mitochondria hypersensitive to aminoglycosides. Even a single dose can trigger rapid, irreversible hearing loss. The T1095C mutation increases gentamicin-induced cell death by 47% compared to normal cells. The OtoSCOPE® genetic test can detect these mutations with 94.7% accuracy. Yet, only a fraction of hospitals use it. In the U.S., just 37% have formal ototoxicity screening protocols. In low-income countries, where aminoglycosides are used most often, testing is virtually nonexistent. This isn’t just a medical gap - it’s a moral one. We have the tools to prevent this damage. But we’re not using them.
Noise, Inflammation, and Other Hidden Risk Factors
Your environment matters. Loud noise doesn’t just add to hearing loss - it multiplies it. Exposure to noise within two months before or after aminoglycoside treatment can increase ototoxicity by up to 52%. Even moderate noise levels - like a busy hospital ward or a loud fan - can push a subtoxic dose into the dangerous zone. Inflammation makes it worse. If you have an infection that triggers endotoxins (like sepsis or pneumonia), those chemicals open the blood-labyrinth barrier wider, letting 63% more aminoglycoside into your inner ear. That’s why patients with urosepsis or TB are at especially high risk. And if you already have high-frequency hearing loss? You’re 3.2 times more likely to lose hearing at lower frequencies too. It’s not just cumulative - it’s compounding.Monitoring Can Save Your Hearing - If It’s Done Right
The good news? We can catch this early. Standard hearing tests (0.25-8 kHz) are too slow. They miss the first signs. High-frequency audiometry (9-16 kHz) detects damage 5 to 7 days earlier. That’s the window where intervention might still help. The American Speech-Language-Hearing Association recommends:- Baseline hearing test within 24 hours of starting treatment
- Monitoring every 48-72 hours during therapy
- Tracking peak and trough drug levels to stay in the therapeutic range

What’s Being Done - And What’s Still Missing
There’s hope on the horizon. The FDA gave Fast Track status to ORC-13661, a drug that protected 82% of hair cells in clinical trials when given with amikacin. Gene therapies targeting mitochondrial mutations are showing promise in mice, reducing ototoxicity by two-thirds. But these aren’t magic bullets. They’re still years away from widespread use. Meanwhile, the World Health Organization reports that 80% of aminoglycoside use happens in places where monitoring, genetic testing, and even basic audiometry are unavailable. The biggest barrier isn’t science. It’s systems. Hospitals don’t have the staff, funding, or protocols. Doctors aren’t trained to ask about hearing. Patients aren’t warned. A 2022 survey of 217 patients found 89% weren’t told about ototoxicity risks before treatment. Most didn’t know their hearing could vanish overnight.What You Need to Know - Before the Next Prescription
If you or someone you care about is being considered for an aminoglycoside - whether for sepsis, TB, or a resistant infection - here’s what to do:- Ask: “Is there an alternative antibiotic?” Sometimes, there is.
- Ask: “Can we do a baseline hearing test before starting?” Insist on it.
- Ask: “Can we test for mitochondrial mutations?” If you have a family history of early hearing loss, this is critical.
- Ask: “Will my hearing be monitored every few days?” If they say no, push back.
- Avoid loud environments during and after treatment. Even normal hospital noise counts.
- Report any ringing in the ears, muffled hearing, or dizziness immediately - don’t wait.
