Diabetes and Heart Disease: How Medications and Lifestyle Together Lower Risk
Dec, 16 2025
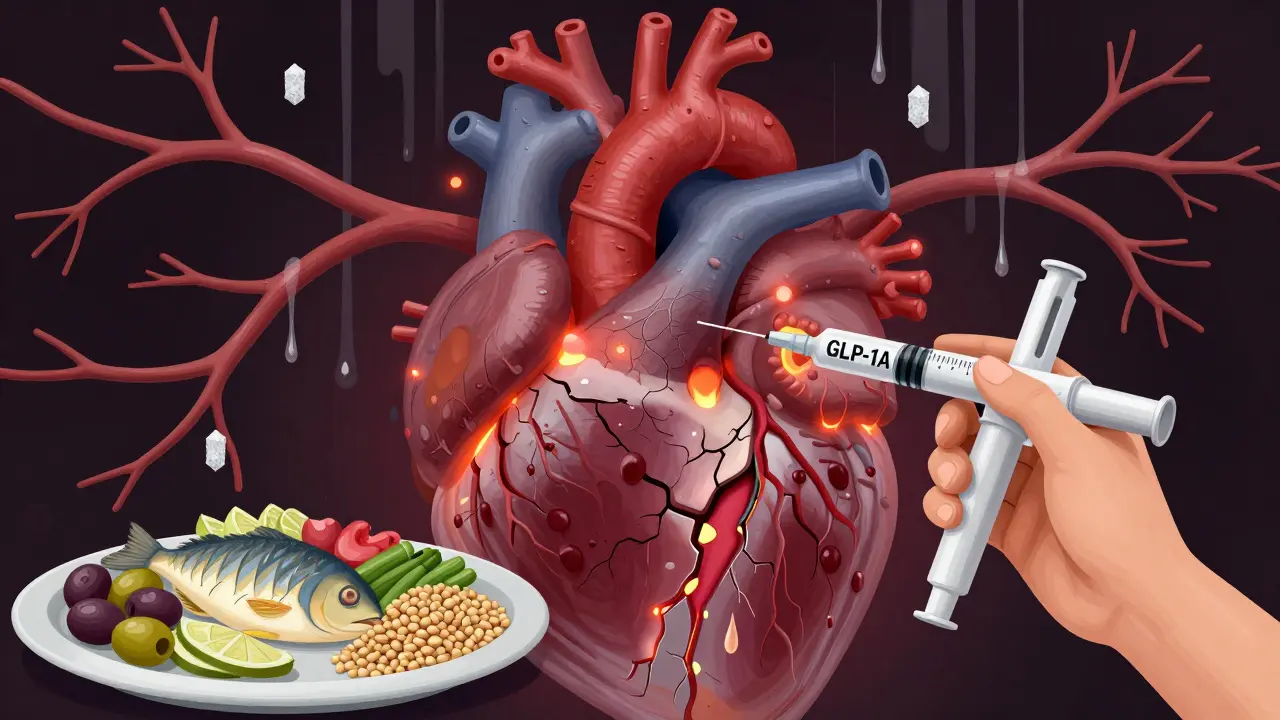
When you have type 2 diabetes, your risk for heart disease isn’t just higher-it’s dominant. About 65% of deaths in people with diabetes are caused by heart problems. That’s not a coincidence. High blood sugar damages blood vessels over time, making them stiff, inflamed, and prone to blockages. But here’s the good news: you don’t have to accept that fate. The latest science shows that combining the right medications with real lifestyle changes can slash your risk of heart attack, stroke, and death-not just a little, but dramatically.
Why Diabetes and Heart Disease Are Linked
Diabetes doesn’t just affect your pancreas. It messes with your whole system. High blood sugar leads to inflammation, raises blood pressure, and increases bad cholesterol (LDL) while lowering good cholesterol (HDL). Fat buildup around your organs-especially belly fat-makes your liver and muscles less sensitive to insulin, which pushes your body into a cycle of more sugar, more fat, and more strain on your heart. The result? Your arteries harden faster. Your heart works harder. Your risk of clots, heart failure, and sudden cardiac events skyrockets.Medications That Do More Than Lower Blood Sugar
For years, metformin was the go-to drug for type 2 diabetes. It helps with blood sugar and has some heart benefits. But now, a new class of drugs is changing the game: GLP-1 receptor agonists. These include semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro, Zepbound). They’re injectables, yes-but they’re not just for weight loss. Semaglutide, at the 2.4 mg weekly dose, helps people lose an average of 14.9% of their body weight. Tirzepatide? Up to 22.5%. That’s not a small number. Losing even 10% of your body weight reduces blood pressure, improves cholesterol, and takes pressure off your heart. But the real breakthrough? These drugs lower the risk of major heart events-like heart attack and stroke-by up to 20% on their own, according to the SELECT and LEADER trials. In 2023, the FDA approved Wegovy specifically for reducing cardiovascular risk in adults with heart disease and overweight or obesity. That’s huge. It’s the first weight-loss drug with an official heart protection label. And it’s not just about the scale. These medications improve insulin sensitivity, reduce liver fat, and calm inflammation-all things that directly protect your heart.Lifestyle Changes That Actually Work
Medications are powerful, but they’re not magic. Real, lasting change comes from how you live. The American Diabetes Association doesn’t give vague advice like “eat better.” They give specifics:- Diet: Focus on Mediterranean, DASH, or plant-based patterns. No need to count carbs obsessively. Eat more vegetables, beans, nuts, whole grains, fish, and olive oil. Cut back on processed meats, sugary drinks, and white bread.
- Movement: At least 30 minutes a day, most days. Break it into 10-minute walks if you need to. Walking after meals helps control blood sugar spikes.
- Blood pressure: Keep it under 130/80 mm Hg. That’s stricter than the general public target.
- Weight loss: Aim for 7% of your starting weight. In the Look AHEAD trial, people who hit that mark saw big drops in blood pressure, triglycerides, and inflammation-even if their heart attack rate didn’t drop dramatically.

The Power of Combining Both
Here’s where it gets really powerful. A study of veterans with type 2 diabetes found something striking: those who took a GLP-1 RA and followed eight heart-healthy habits had a 63% lower risk of major heart events compared to those who didn’t take the drug and didn’t change their lifestyle. That’s not 20% better. That’s more than triple the benefit. Why? Because medications and lifestyle work in different ways. GLP-1 RAs give you a metabolic boost-they help your body burn fat, lower blood sugar, and reduce inflammation. Lifestyle changes fix the root causes: poor diet, inactivity, stress, sleep issues. One handles the chemistry. The other fixes the behavior. The American College of Cardiology made a major shift in June 2025. They now say: don’t make people try lifestyle changes for six months before prescribing these drugs. If you’re overweight and have diabetes or heart disease, you can start the medication right away. But-and this is critical-you still need to add the lifestyle changes. The FDA requires it: Wegovy must be used “in addition to a reduced-calorie diet and increased physical activity.”What About Metformin? Is It Still Enough?
Metformin is still a good first-line drug. It’s cheap, safe, and helps with weight and blood sugar. But compared to GLP-1 RAs, its heart benefits are modest. The LEADER trial showed liraglutide (another GLP-1 RA) reduced major heart events by 13% over placebo. Metformin? Around 10-12% in some studies-but not consistently across all populations. For someone with high risk, that difference matters. If you’re on metformin and still struggling with weight or blood pressure, adding a GLP-1 RA isn’t a sign of failure. It’s a smart upgrade.
Real-World Barriers and How to Get Past Them
These drugs are expensive. Insurance often denies coverage unless you’ve tried other treatments first-or unless you have a BMI over 30 and a related condition like high blood pressure. That’s changing, but slowly. In Australia, Medicare covers Ozempic for diabetes, but not yet for weight loss or heart protection. Out-of-pocket cost can be $1,000+ per month. But here’s the thing: the cost of not acting is higher. A heart attack can cost over $100,000 in treatment and lost income. A stroke? Even more. Prevention saves money-and life. If cost is a barrier, start with lifestyle. Even small changes help. Walk 15 minutes after dinner. Swap soda for sparkling water. Take the stairs. Cut out one processed snack a day. These aren’t glamorous, but they build momentum. Talk to your doctor about generic options, patient assistance programs, or clinical trials. Some pharmacies offer discounts on semaglutide for diabetes use. Don’t give up if you’re denied. Appeal. Ask for a letter of medical necessity.What’s Next?
The field is moving fast. Tirzepatide, a dual GIP/GLP-1 agonist, is showing even stronger results in trials. Combination therapies targeting multiple pathways are being tested. Researchers are building algorithms to predict who will respond best to which drug, based on genetics, fat distribution, and insulin resistance patterns. By 2030, experts predict GLP-1 RAs will be standard for anyone with diabetes and obesity-related heart risk. But the core message won’t change: medication without lifestyle is like putting a bandage on a broken bone. Lifestyle without medication is like trying to fix a leaky pipe with a sponge. Together? They stop the damage.Frequently Asked Questions
Can I stop my diabetes medication if I lose weight with lifestyle changes?
Some people do reduce or even stop diabetes meds after significant weight loss-especially if they’ve lost 10% or more of their body weight and kept it off. But this must be done under medical supervision. Stopping suddenly can cause dangerous blood sugar spikes. Even if your A1C normalizes, your underlying risk for heart disease remains, so ongoing monitoring is essential.
Do GLP-1 RAs cause side effects?
Yes. The most common are nausea, vomiting, diarrhea, and constipation-especially when starting or increasing the dose. These usually improve within weeks. Less common but serious risks include gallbladder disease and pancreatitis. If you have a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia, you should not use these drugs. Always discuss your full medical history with your doctor before starting.
Is it too late to make changes if I already had a heart event?
Never too late. Studies show that even after a heart attack, people who adopt healthy habits and take GLP-1 RAs reduce their risk of another event by up to 50%. Cardiac rehab programs that combine exercise, nutrition counseling, and medication management are among the most effective tools for secondary prevention. The benefits are real, even for older adults.
How long do I need to take these medications?
For most people with diabetes and heart risk, these are long-term treatments-like blood pressure or cholesterol meds. Stopping often leads to weight regain and return of high blood sugar. The goal isn’t to take them forever if you don’t need to, but to use them as tools to build lasting habits. Many people continue them because they feel better, have more energy, and avoid hospital visits.
Can I use these drugs if I don’t have diabetes but have heart disease?
Yes. The SELECT trial showed that semaglutide reduced heart attacks and strokes by 20% in people with obesity and heart disease-even if they didn’t have diabetes. This means the benefits go beyond blood sugar control. If you’re overweight and have heart disease, talk to your doctor about whether this medication could help you, even without diabetes.
