HIV Medications and Antibiotics: What You Need to Know About Dangerous Interactions
Jan, 21 2026
When you’re living with HIV, taking your meds every day is non-negotiable. But what happens when you need an antibiotic for a sinus infection, pneumonia, or a stubborn UTI? It’s not just about popping another pill. Some antibiotics can mess with your HIV treatment in ways that aren’t obvious - and the consequences can be serious.
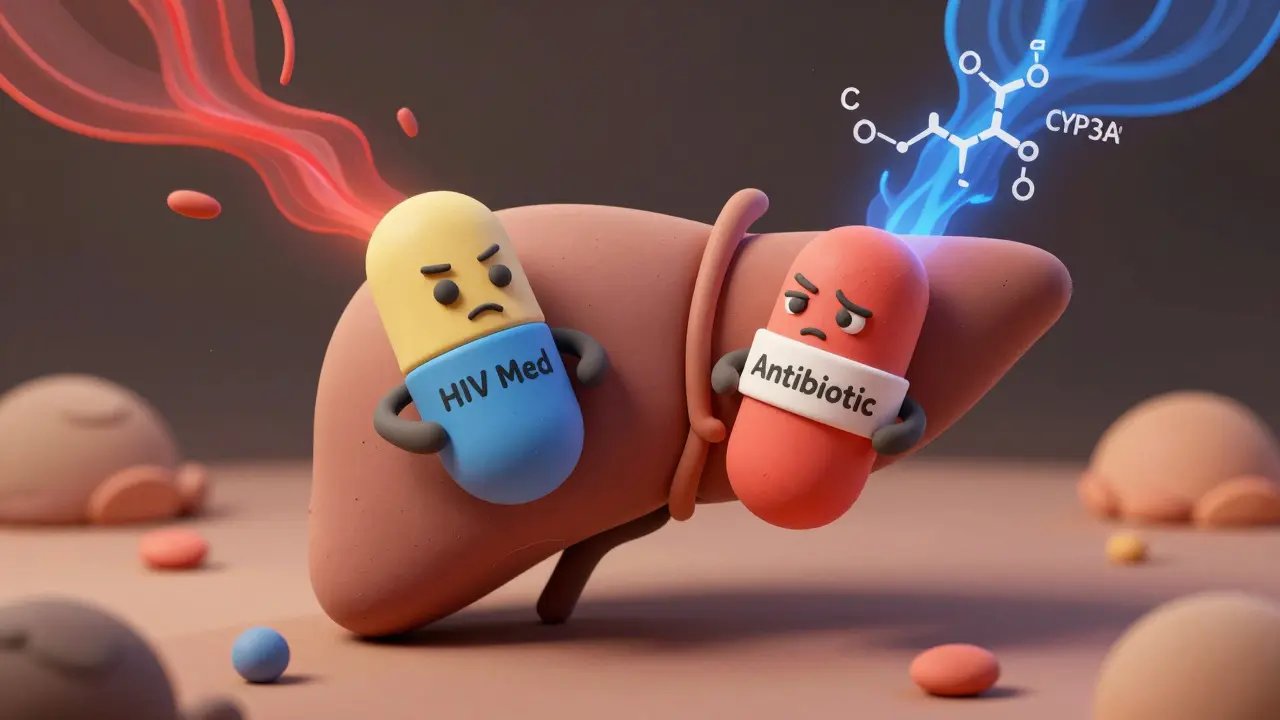
Why HIV Meds and Antibiotics Don’t Always Play Nice
Most HIV medications are processed by your liver using a group of enzymes called cytochrome P450, especially CYP3A4. This is the same system that breaks down a lot of antibiotics. When both types of drugs are in your system at the same time, they can interfere with each other’s metabolism. One might slow down the other’s breakdown, causing toxic levels to build up. Or it might speed it up, leaving you with too little of the drug to keep HIV under control. The problem isn’t random. It’s predictable - if you know where to look. For example, boosted protease inhibitors like darunavir and atazanavir are often paired with ritonavir or cobicistat to boost their levels. But these boosters are powerful CYP3A4 inhibitors. That means they can cause antibiotics like clarithromycin or azithromycin to stay in your body way longer than normal. In one study, clarithromycin levels spiked by 82% when taken with boosted darunavir. That raises your risk of side effects like stomach cramps, irregular heartbeat, or even liver damage. On the flip side, some antibiotics are CYP3A4 inducers. Rifampin, used to treat tuberculosis, is one of the strongest. It can slash HIV drug levels by up to 80%. That’s not just risky - it’s dangerous. A drop in your antiretroviral concentration can lead to treatment failure and drug resistance. That’s why rifampin is outright banned with most boosted HIV meds.Which HIV Drugs Are Most Likely to Cause Problems?
Not all HIV medications are created equal when it comes to interactions. Some are low-risk. Others are ticking time bombs. Nucleoside reverse transcriptase inhibitors (NRTIs) like tenofovir and emtricitabine don’t rely on liver enzymes. They’re mostly cleared by the kidneys. That makes them safer partners for antibiotics. But there’s a catch: tenofovir disoproxil fumarate (TDF) can hurt your kidneys on its own. When you add a fluoroquinolone like ciprofloxacin or levofloxacin, the risk of kidney injury jumps 3.2 times. That’s not a coincidence - it’s additive toxicity. Integrase strand transfer inhibitors (INSTIs) like dolutegravir and bictegravir are the new gold standard for good reason. They’re effective, well-tolerated, and have minimal interactions. Most antibiotics can be safely paired with them. Even trimethoprim-sulfamethoxazole, commonly used for PCP pneumonia, is usually fine - though you’ll need to watch for high potassium levels. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) like efavirenz and rilpivirine are trickier. Efavirenz can lower levels of azithromycin and other macrolides. Rilpivirine, especially in its long-acting injectable form, stays in your system for months. So even if you stop taking it, interactions can linger. Fusion inhibitors like enfuvirtide (now discontinued in the U.S.) and the newer lenacapavir have almost no liver metabolism. That makes them among the safest options if you’re on multiple meds.Antibiotics That Are Safe - and Others to Avoid
Let’s cut through the noise. Here’s what works, and what doesn’t, based on real-world data from the University of Liverpool’s HIV Drug Interactions Database and clinical guidelines updated through 2024.- Safer choices: Azithromycin (for pneumonia or bronchitis), doxycycline (for Lyme or acne), amoxicillin-clavulanate (for sinus infections), and nitrofurantoin (for UTIs) generally play well with most HIV regimens.
- Use with caution: Clarithromycin, erythromycin, and ketoconazole can raise HIV drug levels dangerously. If you must use them, your provider should lower the dose and monitor you closely.
- Avoid entirely: Rifampin (for TB), rifabutin (unless carefully dosed), and voriconazole (for fungal infections) are high-risk. Rifabutin can be used with boosted PIs, but only at 150 mg every other day - and even then, your HIV drug levels will drop by 30-40%.
And here’s a practical tip: if you’re on cobicistat-based regimens (like Biktarvy or Stribild), avoid voriconazole. It can cause severe liver toxicity. Switch to posaconazole instead - it’s just as effective and doesn’t trigger the same reaction.
What You Should Do Before Taking Any New Medication
You don’t need to be a pharmacist to protect yourself. Here’s your simple checklist:- Always tell your doctor you’re on HIV meds. Even if you think it’s just a cold or a rash. Many providers don’t realize how complex these interactions are.
- Check the Liverpool HIV Interactions Database. It’s free, updated monthly, and used by clinics worldwide. Type in your HIV drug and the antibiotic - it’ll tell you if it’s safe, needs a dose change, or is contraindicated.
- Don’t trust pharmacy labels alone. A 2021 study found that Micromedex, Drugs.com, and Liverpool often disagree on whether an interaction is major or minor. Liverpool is the most accurate.
- Ask about alternatives. If your doctor prescribes clarithromycin, ask: “Can I use azithromycin instead?” It’s just as effective for many infections and doesn’t interact with HIV meds.
- Watch for symptoms. If you start feeling dizzy, nauseous, or your heart races after starting an antibiotic, call your provider. It could be a sign your drugs are clashing.

Why This Matters More Than Ever
One in four HIV patients in the U.S. is over 50. That means they’re likely taking meds for high blood pressure, diabetes, or arthritis - plus antibiotics for infections. Polypharmacy isn’t rare. It’s the norm. A 2023 study found that nearly 24% of hospital admissions for HIV patients involved dangerous drug interactions - and antibiotics were behind 41% of those cases. Worse, inappropriate antibiotic use leads to 18% higher readmission rates and a two-fold increase in treatment failure for opportunistic infections. The CDC now lists inappropriate antibiotic use in HIV patients as a key driver of antimicrobial resistance. If your HIV meds are lowered because of a bad interaction, your virus might mutate. Then you’re not just fighting an infection - you’re fighting a drug-resistant strain.What’s Changing in 2025 and Beyond
The field is finally catching up. The NIH launched a $15.7 million project in 2024 to build personalized dosing algorithms using genetic data. New HIV drugs like islatravir show almost no interaction with antibiotics - a game-changer for future regimens. The Liverpool database just rolled out version 10.0 in January 2024, using machine learning to predict new interactions before they’re even published. And by late 2025, major databases like Micromedex and Drugs.com plan to standardize how they classify interactions - ending years of confusion. For now, the best tool you have is awareness. Don’t assume your pharmacist or doctor knows every possible interaction. Be your own advocate. Ask questions. Use the Liverpool tool. And never stop checking - because even a small change in your meds can have big consequences.Can I take amoxicillin with my HIV meds?
Yes, amoxicillin and amoxicillin-clavulanate are generally safe with most HIV medications. They don’t affect the CYP3A4 enzyme system and have no known clinically significant interactions with antiretrovirals. This makes them a preferred choice for bacterial infections like sinusitis or pneumonia in people with HIV.
Is azithromycin safe with boosted HIV drugs?
Yes, azithromycin is one of the safest macrolide antibiotics to use with boosted protease inhibitors like darunavir/ritonavir or atazanavir/cobicistat. Unlike clarithromycin, it doesn’t rely on CYP3A4 metabolism, so it won’t raise HIV drug levels. It’s often the first-line choice for respiratory infections in HIV patients.
What should I do if I’m prescribed rifampin for TB?
Rifampin is contraindicated with most HIV medications because it can reduce antiretroviral levels by up to 80%, leading to treatment failure. If you have TB and HIV, your provider should switch you to rifabutin instead - but even then, the dose must be lowered (150 mg every other day) and your HIV drug levels should be monitored. Never take rifampin with a boosted PI or NNRTI without specialist guidance.
Can antibiotics cause my HIV viral load to rise?
Yes - indirectly. If an antibiotic lowers your HIV drug levels (like rifampin does), your virus can start replicating again. This can cause your viral load to spike and may lead to drug resistance. Even if you don’t feel sick, a rising viral load is a red flag. Always check for interactions before starting any new antibiotic.
Are there any apps or tools to check HIV-antibiotic interactions?
Yes. The University of Liverpool’s HIV Drug Interactions website is the most trusted and accurate tool available. It’s free, updated monthly, and used by clinicians worldwide. You can search by drug name and get instant results on whether an interaction is minor, major, or contraindicated. Avoid using general drug interaction apps - they often miss HIV-specific data.
Should I stop my HIV meds if I need an antibiotic?
Never stop your HIV medications without talking to your provider. Stopping even for a few days can lead to drug resistance and viral rebound. Instead, work with your doctor or pharmacist to find a safe antibiotic alternative or adjust the dose. Most interactions can be managed safely - you just need the right information.
