Cannabis and Medications: What You Need to Know About Drug Interactions
Jan, 30 2026
More people are using cannabis - whether it’s CBD oil for sleep, THC for pain, or full-spectrum products for anxiety - but few realize how deeply it can interfere with their prescription meds. If you’re taking blood thinners, seizure drugs, antidepressants, or even common statins, mixing them with cannabis isn’t just a gray area - it can be dangerous. The science is clear: cannabis doesn’t just sit beside your meds. It changes how your body handles them.
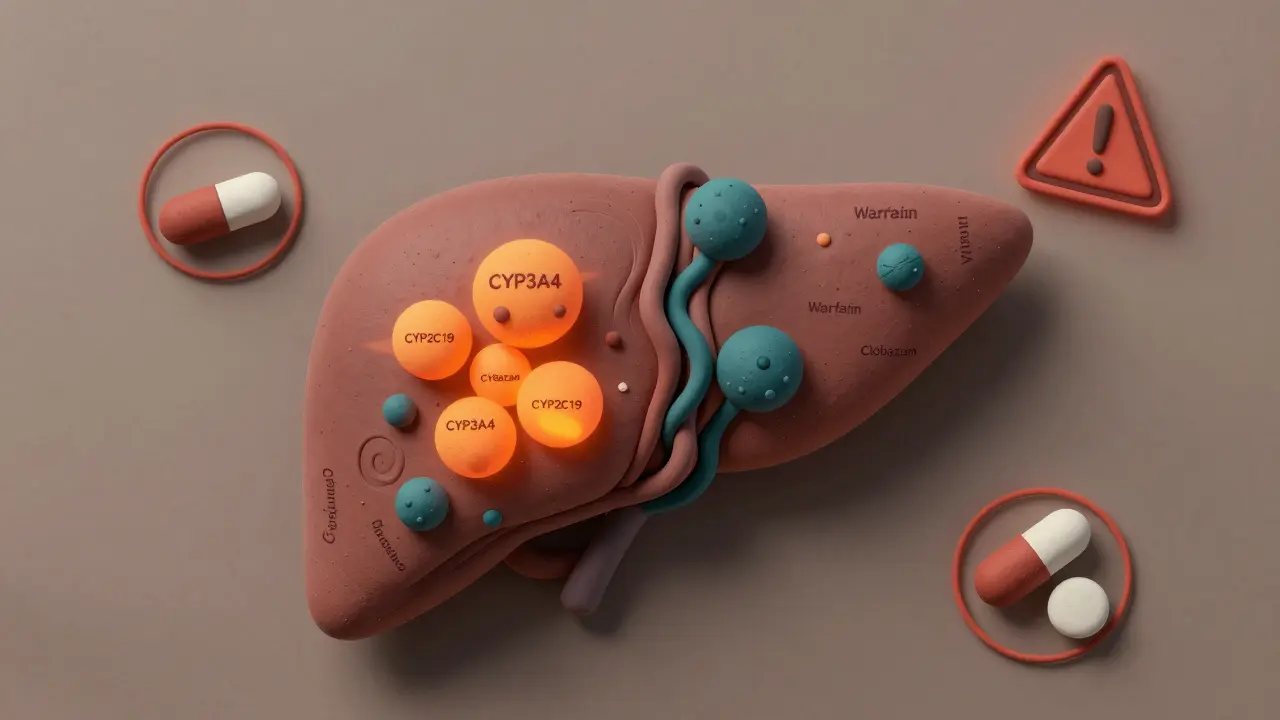
How Cannabis Changes How Your Body Processes Medications
Cannabis doesn’t work like a vitamin or herbal supplement that just floats through your system. Its active compounds - mainly CBD and THC - directly interfere with your liver’s drug-processing system. That system is run by enzymes called cytochrome P450, or CYP450. These enzymes break down about 60% of all prescription drugs. Think of them as the cleanup crew in your body. When CBD or THC shows up, they clog the system. CBD is especially powerful at blocking two key enzymes: CYP3A4 and CYP2C19. THC blocks others, like CYP1A2 and CYP2C9. When these enzymes are inhibited, your meds don’t get broken down as quickly. That means they build up in your bloodstream. For some drugs, that’s harmless. For others, it’s life-threatening. Take warfarin, a blood thinner. A 2022 review of 17 real patient cases found that adding CBD or THC raised INR levels - a measure of blood clotting - by 29% to 48% within just 72 hours. That’s not a small bump. It means your blood takes much longer to clot. One person might end up with unexplained bruising. Another could have internal bleeding. The American College of Clinical Pharmacy documented 12 cases of severe, life-threatening bleeding linked to cannabis and warfarin.High-Risk Medications: Don’t Mix These
Some drugs are simply too risky to combine with cannabis. These aren’t theoretical concerns - they’re documented emergencies.- Warfarin: As mentioned, even a small amount of CBD can push INR levels into dangerous territory. The American Society of Health-System Pharmacists now recommends checking INR every 3-5 days if you’re using cannabis, not once a week like usual.
- Tacrolimus: Used by transplant patients to prevent organ rejection. Cannabis can spike tacrolimus levels by 300% to 500%. That’s enough to cause kidney failure or nerve damage. One case report described a patient who needed emergency dialysis after starting CBD oil.
- Clobazam: An anti-seizure drug. In epilepsy patients, CBD can increase clobazam levels by up to 500%. Many patients end up so sedated they can’t walk. One Reddit user wrote: “I couldn’t walk straight. My neurologist cut my clobazam dose by 40% immediately.”
- Protease inhibitors: Used to treat HIV. THC can reduce their effectiveness by 30% to 40%. That’s not just a side effect - it’s a risk of treatment failure and drug-resistant HIV.
Moderate-Risk Medications: Watch and Adjust
These aren’t absolute no-gos, but they need close attention. You can’t just assume it’s safe because you’ve been using them together for months.- Benzodiazepines (like alprazolam): Both cannabis and these drugs calm the nervous system. Together, they amplify drowsiness, dizziness, and fall risk - especially in older adults. A 2023 study found cannabis use with alprazolam increased fall risk by 47% in seniors.
- Opioids (like oxycodone or morphine): Cannabis slows how fast your body clears these drugs. That means higher levels stay in your blood longer. The result? More sedation, slower breathing, and a higher risk of overdose.
- Calcium channel blockers (like amlodipine): Used for high blood pressure. Cannabis can raise amlodipine levels by 30% to 40%. That can drop your blood pressure too low, causing fainting or dizziness.
Low-Risk Medications: Still, Proceed With Caution
Some meds show only minor changes when mixed with cannabis - but that doesn’t mean they’re risk-free.- SSRIs (like sertraline): CBD may slightly raise sertraline levels by 10% to 15%. Most people feel nothing. But a few report increased anxiety or nausea. If you’re sensitive to meds, start with low-dose CBD and monitor closely.
- Statins (like atorvastatin): CBD can increase atorvastatin levels by 20% to 25%. So far, no cases of muscle damage (rhabdomyolysis) have been confirmed. But if you’re already at risk - say, you’re older or taking other muscle-affecting drugs - it’s not worth the gamble.

It’s Not Just CBD - Formulation Matters
Not all cannabis products are the same. Many people think “CBD isolate” is safer because it has no THC. But that’s not always true. Full-spectrum CBD - the kind with trace THC and other cannabinoids - is actually more likely to cause interactions. Why? The “entourage effect.” When multiple compounds work together, they boost each other’s effects. Research shows full-spectrum products inhibit CYP3A4 enzymes 22% to 37% more than pure CBD isolate at the same dose. Also, how you take it matters. Smoking cannabis? THC hits your blood in 6-10 minutes. That’s a quick, sharp spike - risky if you’re also taking a sedative like Xanax. Oral CBD? It takes 2-4 hours to peak and lasts 6-8 hours. That’s a slow, long-lasting interaction window - perfect for messing with daily meds like warfarin or blood pressure pills.Real People, Real Consequences
Behind the numbers are real stories. A 68-year-old woman in Pennsylvania started taking 25mg of CBD oil for arthritis. She was on warfarin. Two weeks later, she showed up at the ER with a bleeding ulcer. Her INR was 7.8 - normal is 2-3. She’d never bled before. The ER doctor asked about supplements. She mentioned the “hemp oil.” Another patient, a 32-year-old with epilepsy, was doing well on clobazam and CBD. Then he added a new brand of CBD oil - same dose, different company. He woke up unable to stand. His clobazam level had jumped 300%. He needed a hospital stay. But not everyone has problems. One Reddit user took 50mg of CBD daily with oxycodone for eight months with no side effects. That’s why blanket statements don’t work. Your body is unique. Your meds are unique. The product you use is unique.What You Should Do - Step by Step
If you’re using cannabis and take any prescription drugs, here’s what to do:- Be honest with your doctor and pharmacist. Don’t say “I take CBD.” Say: “I take 20mg of full-spectrum CBD oil every night.” Include the brand, dose, and how often.
- Check your meds. Use the University of Washington’s free Cannabis Drug Interactions tool. It’s updated quarterly and lists over 200 medications with known risks.
- Get baseline tests. If you’re on warfarin, tacrolimus, or clobazam, ask for a blood test before starting cannabis. Then test again 48-72 hours after you start.
- Monitor for symptoms. Unusual drowsiness? Bruising? Dizziness? Nausea? These aren’t “just side effects.” They could be signs your drug levels are too high.
- Don’t assume timing helps. Some say take CBD 2 hours apart from your meds. There’s no solid proof this works. The enzymes stay blocked for hours. It’s not about when you take it - it’s about how much you take.

The Bigger Picture
Cannabis use is rising fast. In 2022, over 58 million Americans used it - and 42% of them were also on prescription drugs. Yet only 12 states require pharmacists to counsel patients on interactions. Seventy-six percent of community pharmacists say they feel unprepared to answer these questions. The FDA has started a national clinical trial network to study these interactions. The University of Arkansas is running a $2.3 million study on CBD and warfarin. Results won’t be ready until 2025. Until then, you’re on your own. There’s no magic formula. No one-size-fits-all rule. But there is one truth: if you’re taking a medication with a narrow therapeutic window - meaning the difference between helping and harming is small - cannabis isn’t a harmless add-on. It’s a wild card.Frequently Asked Questions
Can I use CBD if I’m on blood pressure medication?
It depends. CBD can raise levels of calcium channel blockers like amlodipine by 30-40%, which may cause your blood pressure to drop too low. If you’re on a beta-blocker or ACE inhibitor, the risk is lower, but not zero. Start with a low dose of CBD (5-10mg), monitor your blood pressure twice daily for the first week, and talk to your doctor before continuing.
Does smoking cannabis interact differently than CBD oil?
Yes. Smoking cannabis causes a rapid spike in THC, which can intensify sedation if you’re also taking sleep aids, painkillers, or anti-anxiety meds. CBD oil has a slower, longer-lasting effect, which can interfere with daily medications like warfarin or statins over hours or days. The route changes the risk profile - but not the potential for harm.
Is hemp seed oil the same as CBD oil?
No. Hemp seed oil comes from the seeds and contains no CBD or THC. It’s just a nutritional oil - like flaxseed oil. It won’t interact with your meds. CBD oil comes from the flowers and leaves and contains active cannabinoids. If the label says “hemp oil” without mentioning CBD content, it’s likely just seed oil. Always check the lab report.
Can I stop my medication and switch to cannabis instead?
Never stop a prescribed medication without medical supervision. Cannabis isn’t a proven replacement for antiseizure drugs, blood thinners, or HIV treatments. Even if you feel better, stopping your meds could lead to seizures, strokes, or treatment failure. Use cannabis only as an add-on, and only under a doctor’s guidance.
Why do some people say they use CBD with their meds and feel fine?
Because everyone’s body is different. Genetics, liver health, other medications, and even diet affect how your enzymes work. Some people naturally break down drugs faster. Others are slow metabolizers. Just because someone else didn’t have a reaction doesn’t mean you won’t. Your experience is your own.
