Bone-Conduction Hearing Aids: The Alternative Solution for Conductive Loss and SSD

Feb, 4 2026
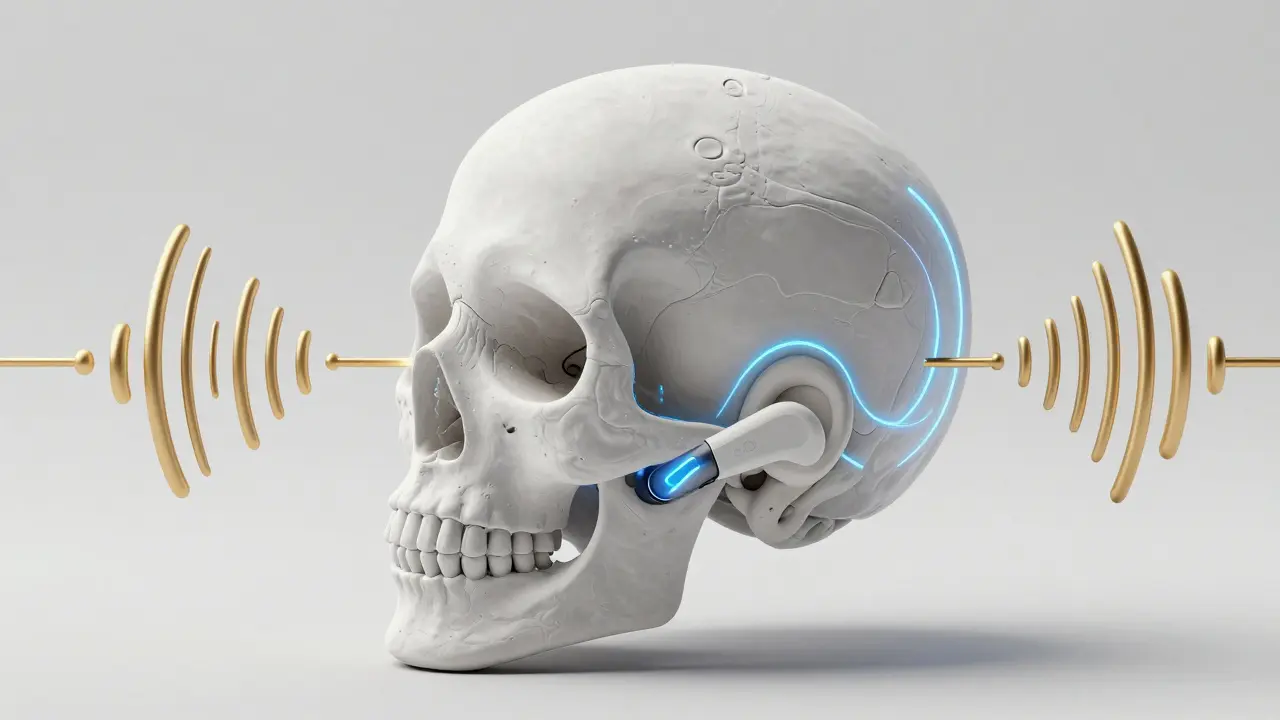
Bone-conduction hearing aids are specialized devices that send sound vibrations directly through the skull bone to the inner ear, bypassing the outer and middle ear entirely. Unlike traditional hearing aids that amplify sound in the ear canal, these devices work by harnessing the natural ability of bone to conduct sound.
For Sarah, a 32-year-old teacher in Sydney, chronic ear infections meant she couldn't use traditional hearing aids. Her left ear was blocked, but her right ear worked fine. Then she discovered bone-conduction hearing aids. Now, she hears birds chirping from both sides. This technology isn't just for the elderly-it's a game-changer for anyone with certain types of hearing loss.
How bone-conduction hearing aids work
The science behind bone-conduction hearing aids dates back to the 1950s. Swedish surgeon Per-Ingvar Brånemark discovered that titanium could fuse with bone tissue. This led to the first Bone-Anchored Hearing Aid (BAHA) system in 1977. Today, these devices transmit sound vibrations directly through the skull to the cochlea. They skip the outer ear and middle ear entirely, making them ideal for people with blocked ear canals or damaged middle ears.
When you wear a bone-conduction hearing aid, the device picks up sound and converts it into vibrations. These vibrations travel through your skull bone, reaching the cochlea directly. This bypasses any problems in the outer or middle ear. For example, if you have a congenital malformation like a missing ear canal, traditional hearing aids won't work. Bone conduction solves that problem.
Who benefits from bone-conduction hearing aids
These devices are designed for three main groups. First, people with conductive hearing loss-where sound can't reach the inner ear due to issues in the outer or middle ear. Second, those with mixed hearing loss, a combination of conductive and sensorineural loss. Third, individuals with single-sided deafness (SSD), where one ear is completely deaf.
For instance, congenital aural atresia (a missing or underdeveloped ear canal) affects about 1 in 10,000 newborns. Traditional hearing aids can't help here, but bone-conduction devices work in 85-90% of cases. Similarly, people with chronic ear infections that make ear canal use impossible find relief. Studies show 92% of chronic ear infection cases can't use regular hearing aids, but bone conduction is a viable option.
Types of bone-conduction hearing aids
There are two main types: percutaneous and transcutaneous systems. Here's how they compare:
| Type | How It Works | Best For | Pros | Cons |
|---|---|---|---|---|
| Percutaneous (e.g., BAHA, Ponto) | Titanium implant with abutment protruding through skin | Severe conductive loss | Higher power output (up to 50 dB), direct sound transmission | Skin complications in 15-30% of cases, requires daily cleaning |
| Transcutaneous (e.g., Bonebridge, BAHA Attract) | Magnetic coupling through intact skin | Single-sided deafness, sensitive skin | No skin irritation, invisible appearance | Lower power (max 45 dB), signal attenuation through skin |
Percutaneous systems like Cochlear's BAHA Connect 6 or Oticon Medical's Ponto 5 SuperPower have a titanium implant that fuses with the skull bone over 3-4 months. The sound processor attaches to an abutment sticking out of the skin. These deliver up to 50 dB of gain but can cause skin issues. Transcutaneous systems like MED-EL's Bonebridge or Cochlear's BAHA Attract use magnets under the skin. They're invisible and avoid skin problems but have slightly less power.
Pros and cons of bone-conduction hearing aids
These devices offer clear advantages. For single-sided deafness patients, studies show 20-35% better speech recognition in noisy environments. They also eliminate the "occlusion effect"-that muffled sound you get when wearing traditional aids in the ear canal. Plus, no ear canal blockage means less discomfort for people with chronic infections or narrow ear canals.
But there are downsides. Percutaneous systems can cause skin reactions in 15-30% of users. For some, this means revision surgery. Transcutaneous systems avoid skin issues but lose 10-15 dB of signal strength through the skin. Both types require minor surgery, which costs $4,000-$7,000 per ear-more than traditional aids ($1,500-$3,500). Also, MRI scans may require implant removal for safety.
User experiences and real-world results
Reddit users on r/Hearing share stories like "Hearing birds chirping from the deaf side for the first time in 15 years" (u/AudiologyNerd, September 12, 2023). A survey on HearGear.com found 65% of users praise the natural sound quality. For those with chronic infections, 82% report freedom from ear canal discomfort.
However, 23% of users on HearingTracker.com complain about MRI incompatibility. Cochlear's 2022 patient registry data shows 28% of BAHA Connect users experience skin reactions, with 8% needing surgery. MED-EL's 2023 survey reports 92% satisfaction with Bonebridge's invisible design compared to 76% for visible abutments.

Market trends and future developments
Currently, bone-conduction hearing aids make up 5.2% of the $12.1 billion global hearing aid market. They're growing faster than traditional aids-8.7% annually versus 4.3%. Cochlear Limited leads with 48% market share, followed by Oticon Medical (27%) and MED-EL (19%). Scandinavia has the highest adoption (1.2% of hearing-impaired Swedes), while the U.S. lags at 0.4%.
New tech is pushing adoption. Cochlear's 2023 BAHA 6 Max includes Bluetooth 5.3 and 30-hour battery life. MED-EL's Bonebridge 3 with AI sound processing launches in Q2 2024. The biggest trend is the shift toward transcutaneous systems, which now represent 63% of new implantations (up from 41% in 2019). Industry analysts predict the market will hit $1.1 billion by 2027, driven by aging populations and improved surgical techniques.
Frequently Asked Questions
Can bone-conduction hearing aids help with chronic ear infections?
Yes. Traditional hearing aids require an ear canal, which is impossible with chronic infections. Bone-conduction devices bypass the ear canal entirely, transmitting sound through the skull. This makes them ideal for 92% of chronic ear infection cases where traditional aids are contraindicated.
How long does surgery take for these devices?
The procedure is outpatient and takes 30-60 minutes under local anesthesia. Percutaneous systems require 3-4 months for osseointegration before activation. Transcutaneous systems can be used immediately after surgery. Most patients return to normal activities within 48 hours.
Are bone-conduction hearing aids covered by insurance?
Coverage varies by country and insurance plan. In Australia, Medicare may cover part of the cost for medically necessary cases. In the U.S., Medicaid and some private insurers cover them for conductive or mixed hearing loss. Always check with your provider before proceeding.
Can I wear glasses with a bone-conduction hearing aid?
Yes, especially with transcutaneous systems. The magnetic coupling doesn't interfere with glasses. Percutaneous systems with abutments may require adjusting the glasses' earpieces, but most users find it manageable. This is a key advantage over traditional in-ear devices.
What's the difference between BAHA and Bonebridge?
BAHA (by Cochlear) is a percutaneous system with a skin-penetrating abutment. Bonebridge (by MED-EL) is a transcutaneous system using magnetic coupling under the skin. BAHA offers higher power output but requires skin care. Bonebridge is invisible and avoids skin issues, though it has slightly lower power. Both are effective for their intended uses.
