Genetic Differences in Drug Metabolism: How Your DNA Affects Medication Safety
When you take a pill, your body doesn’t treat it the same way as everyone else’s. This isn’t about weight, diet, or age—it’s about your genetic differences in drug metabolism, the natural variations in your genes that control how fast or slow your body breaks down medications. Also known as pharmacogenomics, this field explains why some people need half a tablet to feel relief while others need double the dose—and why some get dangerous side effects from drugs that work fine for most.
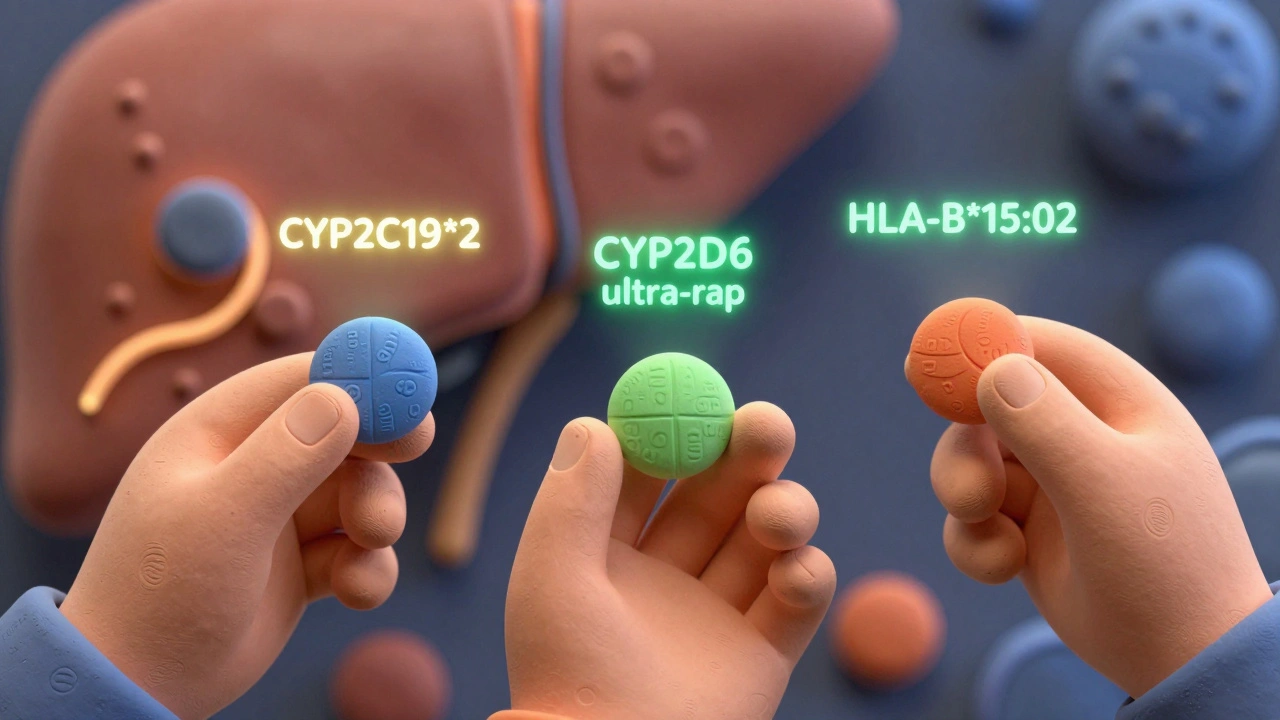
These differences mostly come from enzymes in your liver, especially the CYP450 enzymes, a family of proteins that metabolize over 70% of commonly prescribed drugs. If you have a slow version of CYP2D6, for example, drugs like codeine or tamoxifen won’t convert properly, making them useless—or even harmful. On the flip side, if you’re a fast metabolizer, your body might clear the drug too quickly, leaving you without any benefit. This isn’t rare. About 1 in 5 people have a gene variant that changes how they respond to antidepressants, blood thinners, or painkillers. And it’s not just about effectiveness—it’s about safety. A person with poor CYP2C19 function can bleed dangerously on standard doses of clopidogrel, while someone with ultra-rapid CYP3A4 activity might overdose on certain statins without even knowing it.
These genetic patterns don’t just affect adults. Kids, elderly patients, and people with chronic conditions often have layered risks—like combining a slow-metabolizer gene with kidney trouble or multiple medications. That’s why doctors are starting to test for these variants before prescribing, especially for drugs with narrow safety windows: warfarin, clopidogrel, carbamazepine, and some cancer treatments. The goal isn’t to guess what your body will do—it’s to know. And while genetic testing isn’t routine yet, the data is clear: one-size-fits-all dosing is outdated. Your genes are already telling your body how to handle meds. The question is, are we listening?
Below, you’ll find real-world guides on how these genetic differences connect to everyday medication risks—from QT prolongation and drug interactions to side effects you didn’t expect. These aren’t theoretical discussions. They’re stories from patients and providers who’ve seen firsthand how a simple gene variant changed everything.
Ethnicity and Drug Response: How Genetics Shape Medication Effectiveness
Harrison Greywell Dec, 1 2025 13Ethnicity influences how people respond to medications due to genetic differences in drug metabolism. Learn how CYP enzymes, pharmacogenomics, and ancestry impact drug effectiveness and safety across populations.
More Detail