Preparing for Doctor Appointments: What to Bring and Discuss
Dec, 10 2025
Doctor Appointment Prep Checklist
Your Prepared Checklist
Medications
Symptoms
Questions
Family History
What to Bring to Your Doctor Appointment
Showing up to your doctor’s office without the right things can turn a 15-minute visit into a frustrating, half-hour scramble. You might forget your meds, misremember your symptoms, or walk out without answers because you didn’t ask the right questions. It doesn’t have to be this way.
Start with the basics: medication list. Not just a mental note. Write it down. Include every pill, patch, vitamin, or supplement you take-prescription or not. For each one, note the name, strength (like 10mg or 500mg), how often you take it (e.g., "once daily"), why you take it (e.g., "for high blood pressure"), and who prescribed it. If you’ve been taking something since 2020, write that down too. Mayo Clinic found patients who bring accurate lists have 37% fewer medication errors during visits. That’s not small. It’s life-changing.
Don’t forget your insurance card and a photo ID. Even if you’ve been going to the same clinic for years, they need to verify your details. Some places now require digital check-ins through apps like Cleveland Clinic’s AppointmentPass®, so make sure you’ve logged in and generated your barcode at least 30 minutes before your appointment. If you’re not tech-savvy, show up 15-25 minutes early. Parking, finding the right floor, and waiting in line eat up time faster than you think.
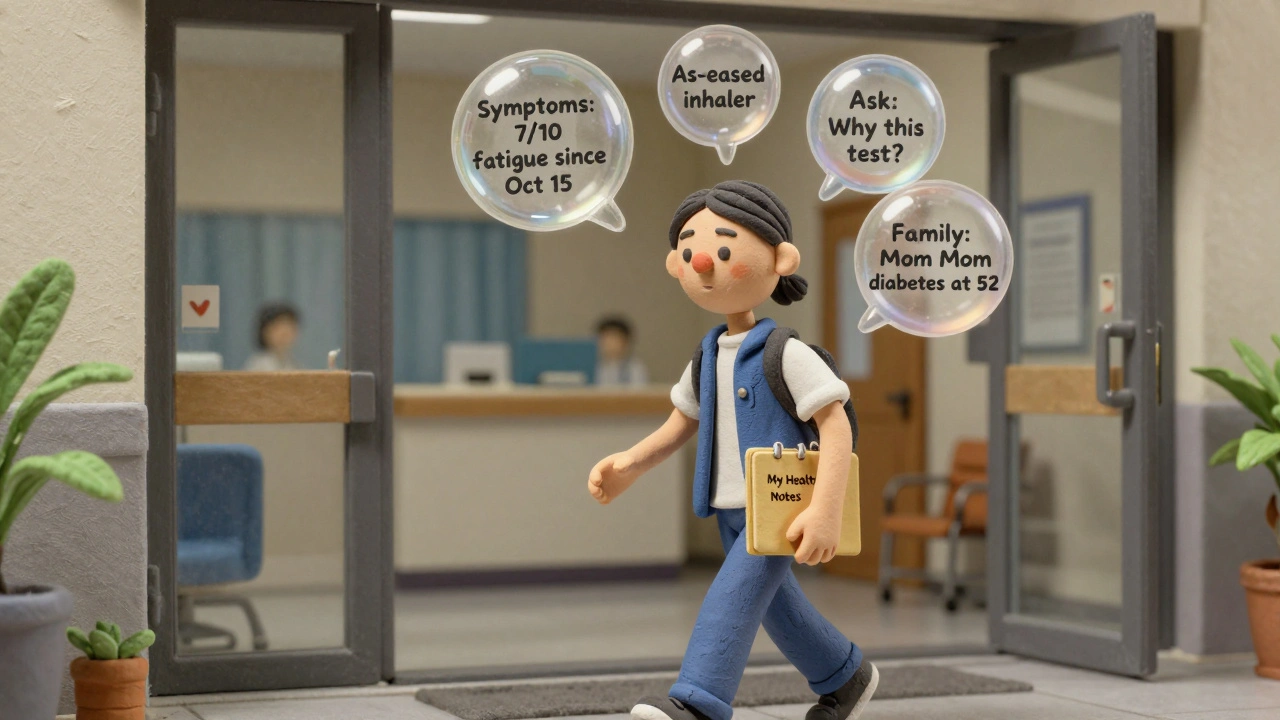
Bring your family health history. Not just "my dad had a heart attack." Be specific: which relatives, what condition, how old were they when it started? For example: "My mother was diagnosed with type 2 diabetes at 52. My paternal grandfather died of a stroke at 68." This helps your doctor spot patterns you might not even realize matter. Mayo Clinic asks for three generations of health data for conditions like cancer, diabetes, and heart disease.
And yes, bring any recent test results or records from other doctors-even if you think they’re irrelevant. A blood test from last month, an X-ray from the ER, or notes from a specialist you saw six weeks ago? Bring them. Your doctor doesn’t have access to every system. You’re the only one who holds the full picture.
What to Discuss: The 12 Critical Topics
Your time with the doctor is short. Don’t waste it on small talk. Go in with a plan. The Institute for Healthcare Improvement recommends focusing on four key areas: medication reconciliation, symptom tracking, goal setting, and follow-up planning. Here’s how to make each one count.
Start with your symptoms. Don’t say "I’ve been tired." Say: "I’ve felt exhausted every day since October 15. It gets worse after lunch. I sleep 8 hours but still wake up drained. On a scale of 1 to 10, it’s a 7 most days." Add what makes it better or worse. Did walking help? Did coffee make it worse? Did you skip your thyroid pill last week? These details turn vague complaints into actionable clues.
Be honest about lifestyle habits. No judgment here-just facts. How much alcohol do you drink? Not "a few drinks," but "two glasses of wine on weekdays, none on weekends." How much exercise? Not "I try to walk," but "I walk 20 minutes, three times a week." Tobacco use? "One pack a day for 18 years." Even if you think it’s embarrassing, your doctor needs to know. AdventHealth’s data shows 68% of patients underreport these things during first visits. That’s a missed chance to catch problems early.
Don’t forget your as-needed medications. People often leave these out. But if you use a rescue inhaler, nitroglycerin, or pain pills for migraines, list them too. These aren’t "extra"-they’re critical. AdventHealth specifically includes them in their protocol because they signal underlying conditions.
And prepare three to five questions you absolutely need answered. Don’t just say "Is everything okay?" Ask: "Why are you recommending this test?" "What are the side effects?" "What would you do if this were your mom?" Cleveland Clinic found patients who bring a prepared question list resolve 89% of their main concerns, compared to 63% for those who don’t.
How to Organize Your Info Before You Go
Don’t wing it the night before. Build a simple system. Use a notebook, your phone’s notes app, or a printable template from your clinic’s website. Here’s a minimal but effective format:
- Medications: Name, Strength, Dose, Purpose, Prescriber, Start Date
- Symptoms: What, When Started, How Often, How Bad (1-10), Triggers, Relief
- Questions: Top 3 you want answered
- Family History: Relative, Condition, Age at Diagnosis
- Lifestyle: Alcohol, Exercise, Smoking, Sleep, Stress
Update this list every time you start or stop a medication. Keep it handy. You’ll use it again next time.
Some clinics now let you upload this info ahead of time. If your doctor uses MyChart, Epic, or another portal, log in a day before and submit your list. Aurora Health Care reports that patients who pre-submit documentation save an average of 14.7 minutes per visit. That’s more time for answers, not paperwork.

Common Mistakes and How to Avoid Them
Most people make the same mistakes. Here’s what not to do:
- Don’t rely on memory. You’ll forget something. Always write it down.
- Don’t skip supplements. Turmeric, fish oil, melatonin-these can interact with meds. Your doctor needs to know.
- Don’t wait until the last minute. Preparing takes 20-30 minutes. Do it the day before. Not the morning of.
- Don’t be afraid to speak up. If you don’t understand something, say so. Ask them to explain it again. No one expects you to know medical jargon.
- Don’t assume your doctor knows your full history. Even if you’ve been seeing them for years, they might not remember every detail. You’re the expert on your own body.
Medication list errors happen in 45% of cases, according to Mayo Clinic. That’s almost half of all patients. A wrong dose, a forgotten pill, a duplicate prescription-it all adds up. Your preparation stops that.
What Happens After the Appointment
The visit isn’t over when you walk out. Write down what your doctor said. If they ordered a test, note when and where. If they changed your meds, confirm the new instructions. Did they say "take once daily"? Double-check the label.
Set a reminder to follow up. If you were told to come back in six weeks, put it in your calendar. If they said "call if symptoms get worse," know what "worse" means. Is it pain going from a 5 to a 7? Is it new dizziness? Define it now.
And if you forgot to ask something? Don’t wait until your next appointment. Many clinics offer secure messaging through patient portals. Send a quick note. Most doctors respond within 48 hours.
Tools and Tech That Help
You don’t have to do this all by hand. Modern tools make it easier:
- MyChart (Cleveland Clinic) lets you import pharmacy data, fill out checklists, and send messages.
- Apple Health and Google Fit can sync your activity, sleep, and even heart rate data-some clinics now pull this in automatically.
- Ambetter Health’s mail-order integration updates your meds automatically when you refill.
- AdventHealth’s LiveWell platform uses AI to suggest questions based on your past visits.
These aren’t gimmicks. They’re built into the system now. If your clinic offers them, use them. 78% of major U.S. healthcare systems now require some form of pre-visit digital prep. You’re not just being helpful-you’re keeping up with the standard.
Why This Matters Beyond Your Appointment
Preparing isn’t just about making your visit smoother. It’s about your long-term health. Studies show patients who prepare regularly have fewer hospital visits, better-controlled chronic conditions, and higher satisfaction with care. It’s not about being perfect. It’s about being consistent.
Every time you bring a clear list, you help your doctor make a better decision. Every time you speak up about your symptoms, you give them the data they need to catch something early. Every time you ask, "What would you do if this were your parent?"-you’re not being difficult. You’re building trust.
This is how you take control. Not with a fancy app or a perfect memory. Just with a notebook, a little honesty, and the courage to ask the hard questions.
What if I forget something during my appointment?
It happens. Don’t panic. Most clinics offer secure messaging through patient portals like MyChart or Epic. Send a quick message after your visit with your question. Many doctors respond within 1-2 business days. If it’s urgent, call the office. Don’t wait until your next appointment.
Do I need to bring my pills in the bottle?
It’s not required, but it helps. If you can, bring your pill bottles or a photo of the labels. This makes it easier for your doctor or pharmacist to verify the name, strength, and instructions. If you use a pill organizer, bring that too-it shows how you’re actually taking your meds, not just what’s on paper.
Should I write down my symptoms before the appointment?
Yes. Write down when they started, how often they happen, how bad they are (use a 1-10 scale), and what makes them better or worse. Don’t rely on memory. Your brain filters out details under stress. Writing them down helps you stay accurate and ensures you don’t leave out key information.
What if I’m nervous about asking questions?
You’re not alone. Most people feel this way. But remember: your doctor expects you to ask questions. The best doctors want you to. Try starting with: "I want to make sure I understand-can you explain this again?" or "What’s the most important thing I should know?" These open the door without pressure.
Is it okay to bring a friend or family member?
Absolutely. Having someone with you helps you remember what was said, ask questions you might forget, and provide emotional support. Just let the clinic know ahead of time so they can make space. Some people even record the visit (with permission) to review later.
