Pharmaceutical Supply Chain Quality: How Poor Logistics Put Patients at Risk

Jan, 27 2026
Cold Chain Temperature Excursion Calculator
Temperature-sensitive medications can lose potency or become ineffective if exposed to improper temperatures. This tool calculates how temperature fluctuations impact drug effectiveness based on the article's data about pharmaceutical supply chain risks.
Enter your medication details and exposure conditions to see how it affects potency.
When you pick up your prescription, you assume the medicine inside is safe, potent, and exactly what your doctor ordered. But what if the path it took to get there-through warehouses, trucks, planes, and delivery vans-was broken? The truth is, the pharmaceutical supply chain is one of the most complex, fragile systems in modern healthcare. And when it fails, patients don’t just wait longer-they suffer, get sicker, or worse.
What Happens When a Drug Doesn’t Stay Cold?
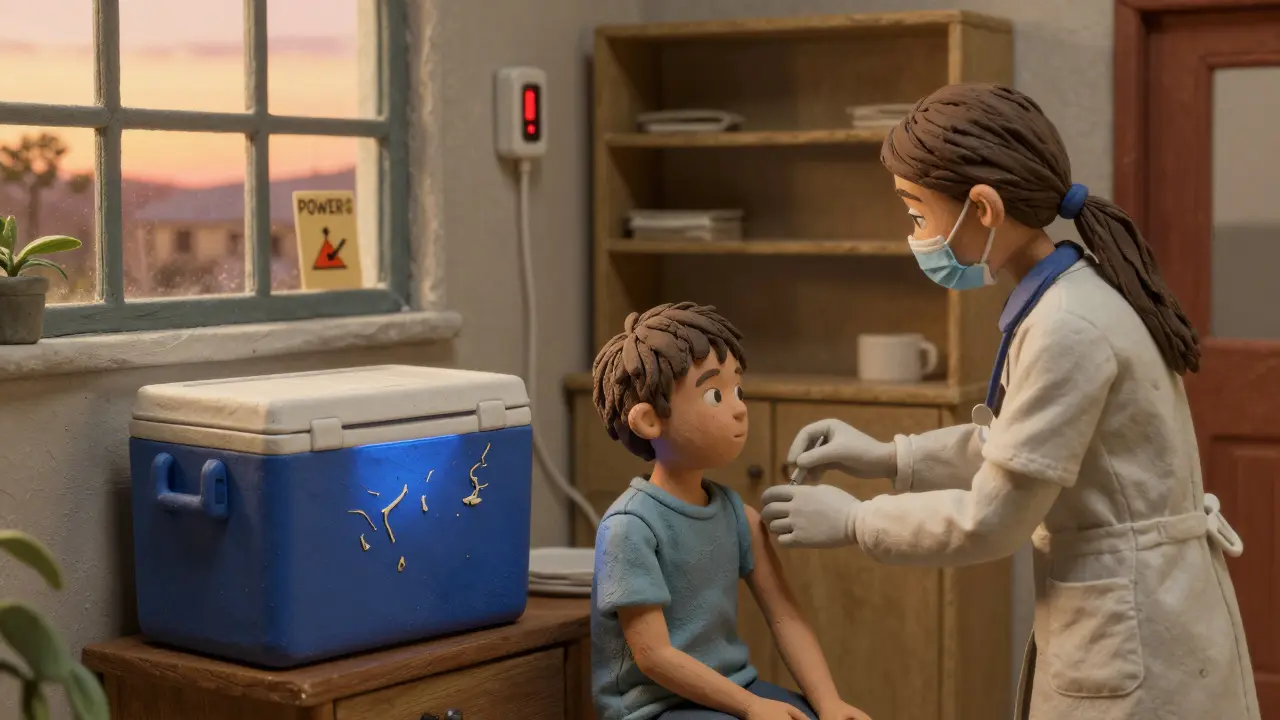
Seventy-two percent of biologic drugs-like insulin, cancer treatments, and vaccines-need to stay between 2°C and 8°C from the moment they leave the factory until they hit your fridge. Fifteen percent need to be kept colder than -60°C. One temperature spike, even for a few hours, can turn life-saving medicine into useless sludge. And it’s not rare. Real-time monitoring shows that 42% fewer temperature excursions happen when companies use digital tracking systems. But not everyone has them. In rural areas, last-mile delivery often means a van without proper cooling, sitting in a hot parking lot for hours. In developing countries, power outages can shut down refrigerated storage for days. The result? Patients get ineffective drugs. A diabetic patient in Jamaica might receive insulin that’s lost its potency. A child in Haiti gets a vaccine that won’t trigger immunity. These aren’t hypotheticals-they’re documented cases tied to supply chain gaps.Counterfeits, Shortages, and the Silent Crisis
Counterfeit drugs aren’t just a problem in shady online pharmacies. They enter legitimate supply chains through compromised distributors, fake serialization codes, or stolen shipments. The FDA’s Drug Supply Chain Security Act (DSCSA), fully enforced by November 2023, requires every prescription drug package to have a unique 2D barcode. That’s a big step. But only 62% of manufacturers were fully compliant by late 2024. The rest? They’re playing catch-up while patients are still at risk. And then there’s the shortage problem. During the first six months of the COVID-19 pandemic, drug shortages jumped 300%. Why? Because 78% of active pharmaceutical ingredients (APIs)-the actual medicine inside pills and injections-are made in just two countries: China and India. When a factory there shuts down for maintenance, a natural disaster hits, or trade tensions flare, the ripple effect reaches every hospital in the U.S., Europe, and Australia. In 2024, Hurricane Helene knocked out Baxter’s North Carolina plant. Over 80% of U.S. hospitals faced shortages of IV fluids, sedatives, and anesthetics. Surgeries were canceled. Patients waited. One Reddit user, a pharmacist in Ohio, posted: “We had three months of epinephrine shortages. We had to ration it for allergic reactions. One kid almost died because we couldn’t get a full dose.”When Substitutions Kill
When a drug is out of stock, pharmacists substitute. It’s legal. It’s common. But it’s dangerous. A 2024 American Hospital Association survey found that 68% of hospitals had to switch medications due to shortages. Of those, 29% reported patients had adverse reactions. Why? Because not all insulin brands work the same. Not all blood pressure pills have identical absorption rates. Not all antibiotics have the same side effect profile. One patient on RateMDs shared: “My Tysabri infusions were delayed 17 days. When I finally got them, my MRI showed two new brain lesions. My neurologist said the gap was likely the cause.” Tysabri isn’t a cold medicine. It’s for multiple sclerosis. A 17-day gap isn’t a minor inconvenience-it’s a medical emergency. Substituting brands without proper monitoring can lead to blood sugar spikes, seizures, organ rejection, or even death. Yet, most hospitals don’t have systems to track how these substitutions affect outcomes. They just hope for the best.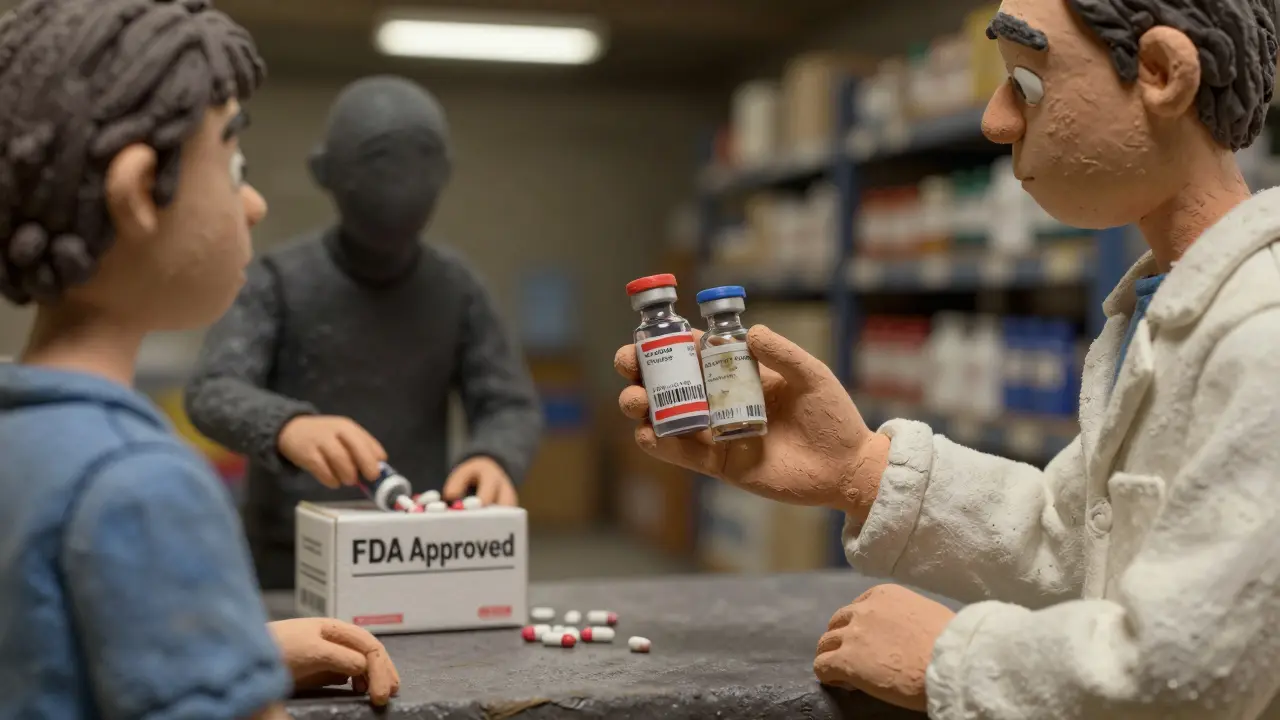
Why the System Is So Fragile
Unlike grocery or electronics supply chains, pharmaceuticals operate with 47% less inventory buffer. Why? Because pills expire. Vaccines spoil. Biologics degrade. You can’t stockpile them like toilet paper. Add to that: 3.2 times more regulatory rules than consumer goods. 217 different compliance standards across major markets. A 12- to 18-month timeline just to implement new tracking systems. And a $2.8 million price tag for a single cold-chain distribution center. Most hospitals can’t afford that. Smaller pharmacies? Forget it. So they rely on big distributors-McKesson, Cardinal Health, AmerisourceBergen-who control 67% of the market. That’s efficient… until one of them has a software glitch. In 2024, a CrowdStrike update crashed systems at 759 hospitals. No inventory data. No order processing. No way to know what drugs were in stock. Emergency rooms were paralyzed.What’s Being Done-and Why It’s Not Enough
Blockchain is being rolled out. AI is being trained to predict demand. Temperature sensors are getting cheaper. The WHO now rates countries on supply chain resilience. These are real advances. But progress is slow. The average hospital takes 8.3 months and $450,000 just to upgrade its tracking system. Staff need 120+ hours of training. Legacy systems from the 1990s still run in half of all U.S. clinics. And cybersecurity? 74% of healthcare breaches in 2023 came from third-party vendors-suppliers, logistics firms, software providers with weak security. Even the best systems fail if they’re not connected. A manufacturer in Germany can track every vial. But if the shipping company in Nigeria doesn’t scan it, or the hospital in rural Kenya can’t read the barcode, the chain breaks. The system works only if every link is strong.