Nodular Acne: Myths Debunked & Facts You Need to Know

Sep, 22 2025
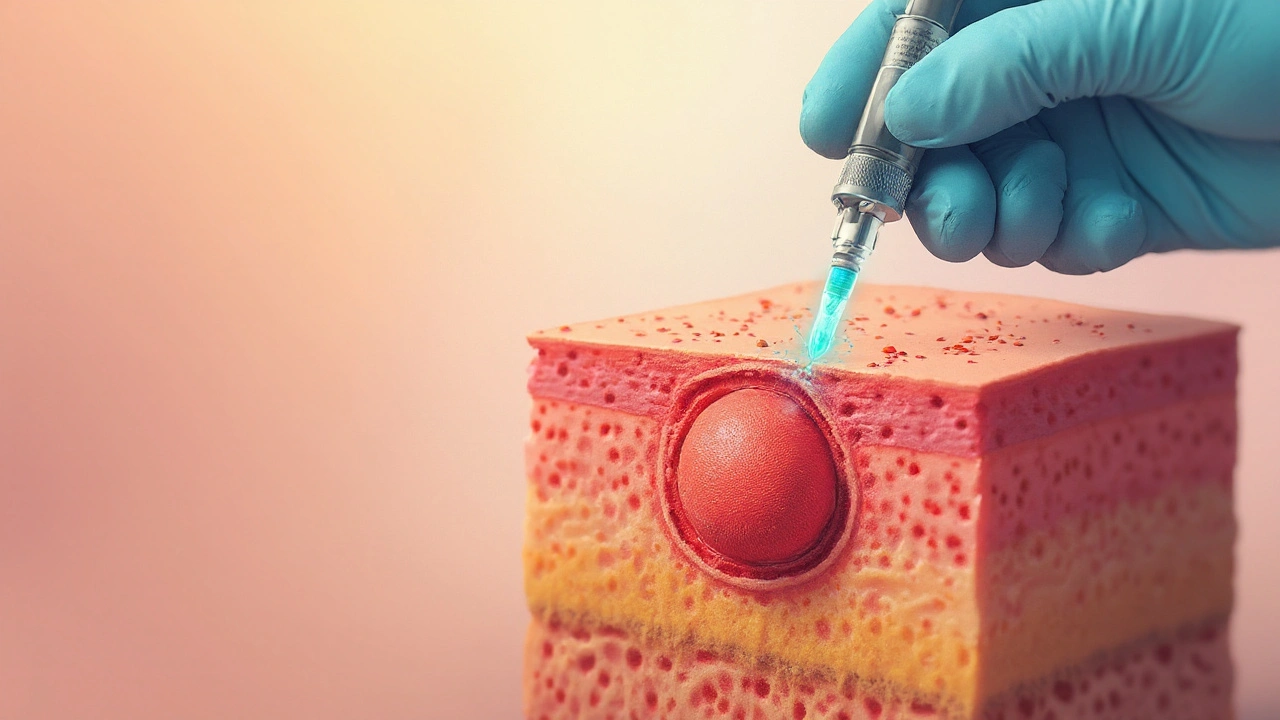
Nodular acne is a severe form of acne characterized by large, inflamed, painful bumps that develop deep within the skin. These nodules often feel like hard pebbles and can leave lasting scars if untreated. Understanding what drives them is the first step toward wiping them out.
What Makes Nodular Acne Different?
At its core, nodular acne is a subtype of acne vulgaris the most common skin condition affecting up to 85% of teenagers and many adults. While whiteheads and blackheads sit near the skin surface, nodules form when the follicular wall ruptures, spilling oily sebum, dead cells, and bacteria into surrounding tissue. This triggers a cascade of inflammation driven by androgen hormones male‑type hormones such as testosterone that increase sebum production and the activity of the sebaceous gland oil‑producing units attached to each hair follicle. The combination of excess oil, clogged pores, and Cutibacterium acnes formerly Propionibacterium acnes, a skin‑resident bacterium that thrives in oily environments fuels the deep inflammation that creates nodules.
Top Myths About Nodular Acne
- Myth: "Nodules are caused by dirty skin." Fact: Even the cleanest skin can develop nodules if excess sebum and hormonal spikes push the follicle over the breaking point.
- Myth: "Only teenagers get nodular acne." Fact: Adults, especially women in their 20s‑30s, can experience hormonal fluctuations that trigger nodules.
- Myth: "Popping or squeezing will cure it." Fact: Squeezing ruptures the follicle further, spreading inflammation and scarring.
- Myth: "Over‑the‑counter creams are enough." Fact: Mild topicals may help comedonal acne, but nodular acne often requires prescription‑strength medication.
- Myth: "Stress alone causes nodules." Fact: Stress can exacerbate hormone levels, but it’s one of many contributors, not the sole cause.
Evidence‑Based Facts You Should Trust
Professional guidelines from the American Academy of Dermatology and Australian Skin Cancer Foundation agree on three pillars for managing nodular acne:
- Reduce inflammation quickly to prevent tissue damage.
- Control bacterial overgrowth without encouraging resistance.
- Regulate sebum production for long‑term stability.
These pillars translate into specific treatment choices, each with proven efficacy in clinical trials involving thousands of participants. For instance, a 2023 multicenter study found that isotretinoin an oral retinoid that normalizes skin cell shedding and dramatically reduces sebum output achieved clear skin in 85% of patients with severe nodular acne after a 16‑week course.
Choosing the Right Treatment: A Quick Comparison
| Therapy | Mechanism | Typical Duration | Common Side Effects |
|---|---|---|---|
| Isotretinoin | Reduces sebaceous gland size & sebum, normalizes keratinisation | 4-6 months | Dry skin, cheilitis, elevated liver enzymes |
| Topical Retinoid | Promotes cell turnover, prevents comedo formation | 12-24 weeks | Irritation, peeling, photosensitivity |
| Oral Antibiotic | Suppresses Cutibacterium acnes, anti‑inflammatory | 6-12 weeks | Gastrointestinal upset, resistance risk |
How a Dermatologist Guides Your Journey
Seeing a dermatologist a medical specialist trained to diagnose and treat skin disorders is crucial for nodular acne. They can assess lesion depth, order blood work to rule out hormonal imbalances, and prescribe systemic therapies that you can’t obtain over the counter. Many doctors also combine treatments-e.g., starting isotretinoin while using a gentle topical retinoid to smooth the skin’s texture.
Related Factors That Influence Nodular Acne
Even with optimal medication, lifestyle and secondary skin‑care habits affect outcomes:
- Diet: High glycaemic load foods (white bread, sugary drinks) may spike insulin, indirectly increasing androgen activity.
- Stress management: Chronic cortisol elevation can amplify androgen production, worsening lesions.
- Skin barrier health: Over‑exfoliating or harsh cleansers strip protective lipids, allowing irritants to penetrate deeper.
- Scarring prevention: Early intervention with silicone gels or laser resurfacing reduces permanent marks.
These variables sit alongside the primary biological drivers and should be addressed in a holistic treatment plan.
What to Expect During Treatment
Most patients notice a reduction in redness and swelling within the first 2-4 weeks of starting isotretinoin or a potent oral antibiotic. However, complete resolution can take several months, and occasional flare‑ups are normal as the skin adjusts. Regular follow‑up appointments allow the dermatologist to monitor liver function, lipid levels, and mood changes-especially important for isotretinoin users.
When to Seek Immediate Help
If you experience any of the following, contact your doctor right away:
- Sudden, severe facial swelling or pain
- Fever or chills (signs of infection)
- Vision changes or eye involvement
- Unexplained mood swings while on isotretinoin
Prompt treatment can prevent deep tissue damage and permanent scarring.

Frequently Asked Questions
Can I use over‑the‑counter acne products while on prescription treatment?
Yes, but choose gentle, non‑comedogenic formulas. Harsh scrubs or high‑alcohol toners can irritate already inflamed skin and reduce the effectiveness of prescription meds.
How long does isotretinoin therapy usually last?
A typical course runs 4-6 months, aiming for a cumulative dose of 120-150mg/kg body weight. Some patients may need a second round if nodules recur.
Is nodular acne contagious?
No. The condition stems from internal hormonal and inflammatory processes. While the bacteria involved are normal skin flora, they don’t spread through casual contact.
Will diet changes cure my nodular acne?
Diet alone rarely cures severe acne, but reducing high‑glycaemic foods and increasing omega‑3 fatty acids can support treatment and lessen flare‑ups.
Are there natural remedies that work?
Some botanical extracts (tea tree oil, niacinamide) show modest anti‑inflammatory benefits, but they should complement-not replace-doctor‑prescribed therapy for nodular lesions.
Can hormonal birth control help women with nodular acne?
Combination oral contraceptives that contain estrogen can lower androgen levels and often improve acne severity in many adult women.
What’s the best way to prevent scarring?
Start treatment early, avoid picking, and discuss early scar‑modulation options (silicone sheets, laser therapy) with your dermatologist.
