Hormone Replacement Therapy and Drug Interactions: What You Need to Know

Nov, 22 2025
HRT Drug Interaction Checker
Check Your Medications
Enter medications you're taking and see how they interact with hormone replacement therapy (HRT).
When you start hormone replacement therapy (HRT) for menopause, you’re not just adding one medication to your routine-you’re changing how your whole body processes everything else you take. Many women don’t realize that the estrogen or progestin in their HRT can make their epilepsy meds less effective, interfere with thyroid tests, or even reduce the power of antidepressants like lamotrigine. These aren’t rare side effects. They’re well-documented interactions, and they can be dangerous if no one is watching.
How HRT Changes How Your Body Handles Other Drugs
HRT doesn’t just sit there. It actively changes how your liver works. Estrogen, especially in pill form, tells your liver to make more enzymes-specifically UGT1A4-that break down other drugs faster. That means medicines like lamotrigine, used for epilepsy and depression, get cleared out of your system before they can do their job. A case reported by the Netherlands Pharmacovigilance Centre Lareb in 2022 showed a woman’s lamotrigine levels dropped sharply after starting Femoston (estradiol/dydrogesterone). Her depression worsened. When she stopped HRT, her levels came back up. That’s not a coincidence. That’s a direct interaction.
It’s not just lamotrigine. Anticonvulsants like carbamazepine and phenytoin, antibiotics like rifampicin, and even HIV meds can be affected. The same liver enzymes that break down estrogen also speed up the breakdown of these drugs. The result? Lower blood levels. Reduced effectiveness. More symptoms. More risk.
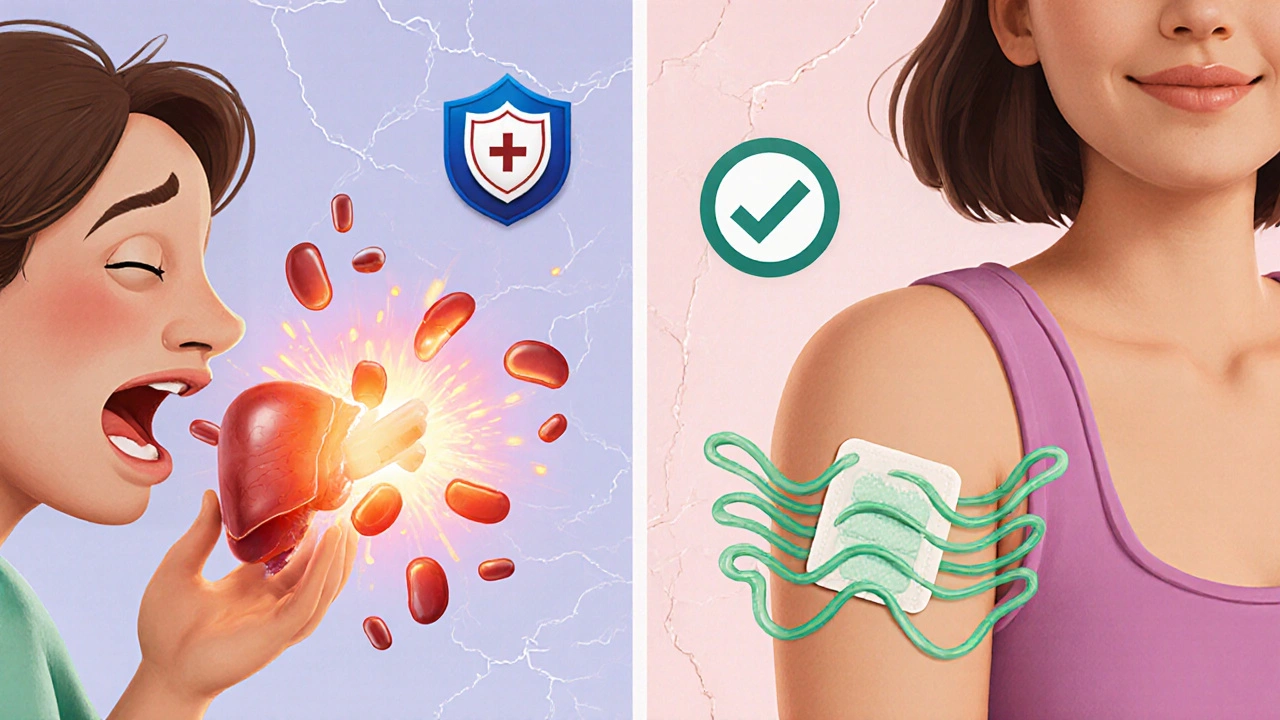
Transdermal Patches vs. Pills: A Major Difference
If you’re on HRT and worried about interactions, the delivery method matters more than you think. Oral HRT-tablets and capsules-goes straight to your liver on the first pass. That’s where the enzyme activity spikes. Transdermal patches, gels, or sprays? They bypass the liver. The hormones enter your bloodstream through your skin. That means much less impact on liver enzymes.
The NHS confirms this: patches are less likely to interfere with other medicines. If you’re taking St. John’s wort, for example, it can make oral HRT less effective. But patches? They’re mostly unaffected. The same goes for epilepsy meds, thyroid drugs, and blood thinners. If you’re on multiple medications and your HRT isn’t working as expected, switching from pills to patches might be the simplest fix.
Interactions You Might Not Realize Are Happening
Some interactions don’t cause obvious symptoms. They mess with your lab tests instead. If you’re on hydrocortisone for adrenal insufficiency and start HRT, your cortisol blood levels will look higher-not because you have more active hormone, but because estrogen increases a protein called corticosteroid-binding globulin (CBG). That protein binds to cortisol, making it inactive. Your total cortisol goes up, but your free, active cortisol? It’s unchanged. If your doctor relies on total cortisol to adjust your dose, you could end up under-treated. You need a free cortisol test instead.
Even herbal supplements can cause trouble. St. John’s wort is the most documented. It’s sold as a natural mood booster, but it’s a strong liver enzyme inducer. It can reduce HRT effectiveness by up to 50% in some cases. The NHS explicitly warns against it. Resveratrol, found in red grapes and supplements, has a chemical structure similar to synthetic estrogen. While evidence is weak, it’s not zero. And rosemary? One study suggests it might speed up estrogen breakdown. Not enough to rely on, but enough to be cautious.
Who’s at Highest Risk?
Not everyone on HRT needs to panic. But certain people need extra attention:
- Those taking medications with a narrow therapeutic index-like warfarin, lithium, or lamotrigine. A small drop in blood level can mean a big drop in control.
- Women with epilepsy. Estrogen can lower seizure thresholds, and if your anticonvulsant levels drop, seizures can return.
- People on thyroid replacement. Estrogen increases thyroid-binding proteins, which can make your TSH levels look off. Your doctor may need to adjust your levothyroxine dose.
- Those taking testosterone alongside hydrocortisone. This combo can cause fluid retention-swollen hands, feet, ankles. Watch for it.
The NIH warns that with any drug, there’s potential for interaction-but it’s especially critical when you’re on HRT and something with a narrow window between effective and toxic doses.
What to Do Before Starting HRT
Don’t wait until something goes wrong. Before you begin HRT, make a full list of everything you take:
- All prescription drugs
- All over-the-counter meds
- All vitamins, minerals, and supplements
- All herbal remedies-including teas and tinctures
Bring this list to your doctor. Don’t assume they know. Don’t assume it’s harmless. Tell them you’re considering HRT and want to know about interactions. If your doctor doesn’t know the answer, ask for a referral to a pharmacist who specializes in drug interactions. Pharmacists are trained to spot these things. They’re the ones who catch the lamotrigine-HRT link before it hurts someone.
What to Watch For After Starting
Pay attention to changes in the first few months:
- Are your seizures more frequent?
- Is your mood worse, even if you started HRT for better sleep and hot flashes?
- Do you feel your thyroid meds aren’t working as well?
- Are you suddenly swollen in your hands or feet?
- Have you developed a severe headache, vision changes, or trouble speaking?
These aren’t normal menopause symptoms. They’re red flags. Call your doctor immediately if any of these happen. The European regulatory update in 2022 came from a single case report. That’s how these things are found-by patients and doctors noticing something off.
When to Pause HRT
If you’re scheduled for surgery, or you’ll be bedridden for more than a few days, your doctor should tell you to stop HRT at least 4 to 6 weeks beforehand. Why? Because estrogen increases your risk of blood clots. If you’re immobile, that risk skyrockets. This applies even if you’re young and healthy. It’s not about age-it’s about movement.
Same goes if you develop new high blood pressure, a history of blood clots, or signs of breast cancer. HRT isn’t something you take forever unless you absolutely need it. The goal is symptom relief at the lowest dose for the shortest time. That’s the standard. If you’ve been on it for 5 years without a review, it’s time to ask: Do I still need it?
The Bottom Line
HRT works. It helps with hot flashes, night sweats, sleep, and mood. But it’s not a simple pill. It’s a system changer. It alters your liver’s behavior, your hormone balance, and how your body handles other medicines. Many women suffer in silence because they don’t realize their worsening depression or seizures might be tied to HRT-not their condition.
Don’t assume your doctor knows every interaction. Don’t assume herbal remedies are safe. Don’t assume patches and pills are the same. Ask. Track. Report. Your body is telling you something. Listen.
Can HRT make my epilepsy worse?
Yes. Estrogen in HRT can lower your seizure threshold, and if it causes your anticonvulsant medication (like lamotrigine or carbamazepine) to break down faster, your seizure control can decline. A 2022 case from the Netherlands showed a woman’s lamotrigine levels dropped by over 40% after starting HRT, leading to a return of depressive symptoms and seizure activity. If you have epilepsy, discuss your HRT options with a neurologist and consider transdermal patches, which are less likely to interfere.
Is it safe to take St. John’s wort with HRT?
No. St. John’s wort strongly activates liver enzymes that break down estrogen and progestin. This can reduce HRT effectiveness by up to half, making hot flashes and other symptoms return. It can also interfere with other medications like antidepressants or birth control. The NHS and multiple clinical guidelines warn against combining them. If you’re using it for mood, talk to your doctor about safer alternatives.
Why does my cortisol level look high on blood tests after starting HRT?
Estrogen increases a protein called corticosteroid-binding globulin (CBG), which binds to cortisol in your blood. This makes your total cortisol reading rise, but your active, free cortisol stays the same. If you’re on hydrocortisone for adrenal issues, your doctor can’t use total cortisol to adjust your dose. You need a free cortisol test or an ACTH stimulation test instead. Otherwise, you might be under-treated.
Do I need to stop HRT before surgery?
Yes, if you’re having major surgery or will be immobile for more than a few days. Estrogen increases your risk of blood clots. The standard recommendation is to stop oral HRT 4 to 6 weeks before surgery. Patches may be safer, but your surgeon will still likely ask you to pause them. This isn’t optional-it’s a safety rule for anyone on estrogen, regardless of age or health.
Are bioidentical HRT products safer in terms of interactions?
No. Bioidentical HRT-often marketed as natural or safer-is still made of estrogen and/or progesterone. Whether it’s synthetic or plant-derived, the molecules are identical to your body’s hormones. That means they interact with the same liver enzymes and medications. There’s no evidence they’re safer or cause fewer interactions. The same warnings about lamotrigine, St. John’s wort, and blood clots apply.
Can HRT affect my thyroid medication?
Yes. Estrogen increases thyroid-binding proteins, which can make your TSH levels appear higher than they are. This might lead your doctor to increase your levothyroxine dose unnecessarily. If you start HRT and your thyroid levels seem off, ask for a free T4 test and TSH together. You may need a dose adjustment, but only after confirming your actual hormone levels-not just the total thyroid binding.
Next Steps: What to Do Today
If you’re on HRT and any other medication, take 10 minutes right now:
- Write down every drug and supplement you take.
- Check if any are anticonvulsants, blood thinners, thyroid meds, or St. John’s wort.
- If yes, call your doctor or pharmacist and say: “I’m on HRT. Could any of these interact?”
- If you’re on pills and worried, ask about switching to patches.
- If you’ve had unexplained worsening symptoms since starting HRT, don’t ignore it. It might not be your condition-it might be your meds.
HRT is powerful. It helps millions. But it’s not harmless. The best outcomes come from knowing how it works-not just what it does.
