Constipation: Causes, Laxatives, and How to Manage It Long-Term
Dec, 1 2025
Constipation isn’t just about not going to the bathroom often-it’s about struggling to pass hard, dry stools, feeling like you haven’t fully emptied your bowels, or needing to strain too much. If you’re going fewer than three times a week and it’s been happening for weeks or months, you’re not alone. About one in three people who see a doctor for gut issues are dealing with constipation. In the U.S. alone, over 2.5 million people seek medical help for it every year. The good news? Most cases can be managed effectively-if you know what’s really going on.
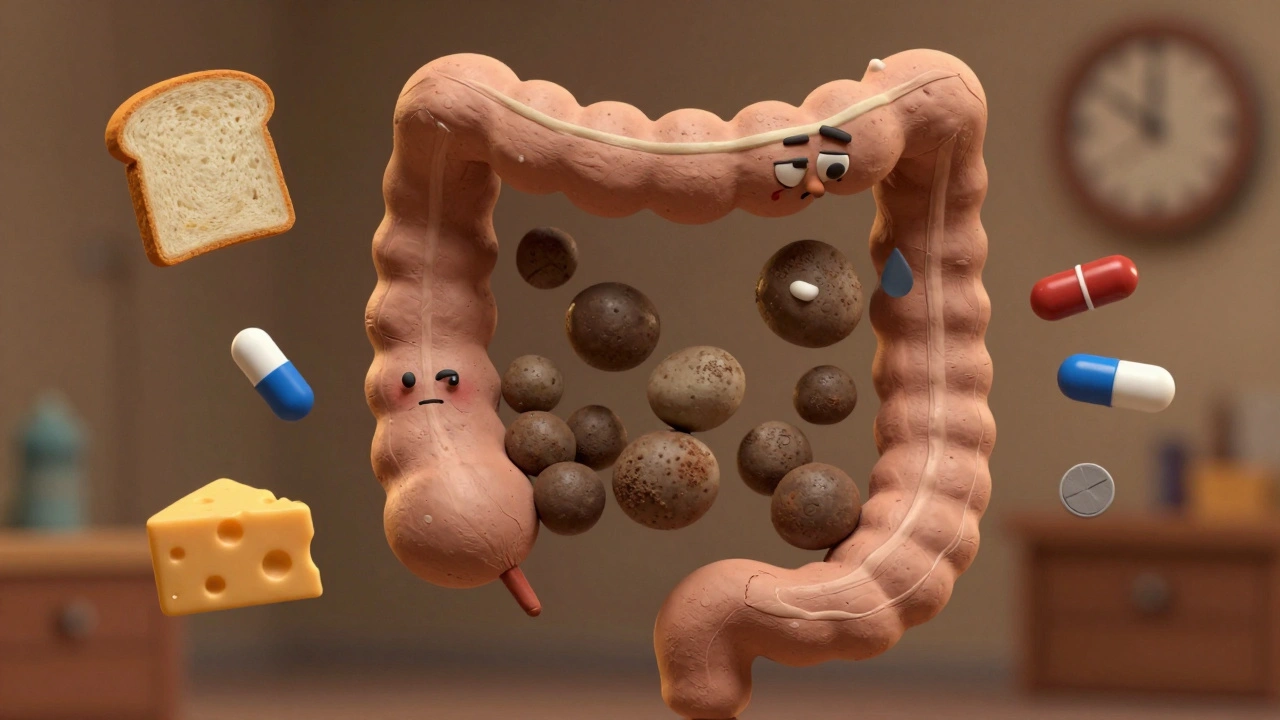
What’s Actually Happening in Your Body?
Your colon is supposed to move waste along at a steady pace, usually within 24 to 72 hours. But in constipation, that process slows down. Water gets sucked out of the stool as it sits too long, turning it into hard, pebble-like chunks. That makes it tough to push out. It’s not just about diet-though that plays a big role. The real problem often lies in how your muscles and nerves work together. Some people have slow-moving colons. Others have pelvic floor muscles that don’t relax properly when they try to go. That’s called a defecatory disorder. And then there are those whose colon moves fine, but they still feel blocked or incomplete after trying. That’s normal transit constipation, the most common type.Why Does This Happen? The Real Causes
You might blame your diet, and yes, low fiber and not drinking enough water are big factors. Most Americans eat only about 15 grams of fiber a day-half the recommended 25 to 30 grams. But there’s more to it. Many people don’t realize that medications can be the hidden culprit. Opioids, like painkillers, cause constipation in up to 95% of long-term users. Calcium channel blockers for high blood pressure, tricyclic antidepressants, and even iron supplements can slow things down. If you started a new drug and noticed changes in your bowels, that’s likely why. Medical conditions also play a major role. Nearly 60% of people with diabetes have constipation. So do 50 to 80% of those with Parkinson’s disease. Hypothyroidism, multiple sclerosis, and spinal cord injuries are also common triggers. Age matters too. After 60, your risk goes up by about 1.5% each year. Women are more likely to struggle with it than men-67% of patients are female. And if you’ve had a stroke, are on dialysis, or have heart disease, your odds go up even more.What Laxatives Actually Work (And Which Ones Don’t)
There are dozens of laxatives on the shelf, but not all of them do what they promise. Here’s what science says about the most common types:- Bulk-forming laxatives (like psyllium or methylcellulose) are great for most people. They soak up water and make stool bigger and softer, which triggers natural contractions. But they only work if you drink enough water-8 ounces per dose, minimum. If you don’t, they can make constipation worse.
- Osmotic laxatives (like PEG 3350, lactulose, magnesium hydroxide) pull water into the colon. PEG 3350 is the gold standard. It works for 65 to 75% of people, has almost no side effects at normal doses (17g daily), and is safe for long-term use. It’s what doctors recommend first.
- Stimulant laxatives (senna, bisacodyl) force your intestines to contract. They work fast-often in 6 to 12 hours-and are effective for short-term relief. But using them longer than 12 weeks can damage your colon’s natural ability to move stool. That’s called cathartic colon. Avoid them unless you’re under a doctor’s supervision.
- Stool softeners (docusate sodium) are popular, but studies show they’re barely better than a placebo. Don’t rely on them alone.
- Prescription options like linaclotide, lubiprostone, and plecanatide are for stubborn cases. They work by increasing fluid in the gut. They’re expensive but can be life-changing for people who’ve tried everything else.

Long-Term Management: Beyond Pills
Relying on laxatives forever isn’t the goal. Real relief comes from fixing the root problem. Here’s how:- Boost fiber slowly. Add 5 grams of fiber every 3 to 4 days. Jumping from 15g to 30g overnight will make you bloated and gassy-30 to 40% of people experience this. Focus on soluble fiber: oats, beans, apples, chia seeds, and psyllium husk. It holds water better than insoluble fiber.
- Drink more water. For every 5 extra grams of fiber, add another 250 to 500 mL of water. Aim for 1.5 to 2 liters daily. If you’re on fiber and still constipated, you’re probably not drinking enough.
- Train your body to go. Sit on the toilet for 10 to 15 minutes after breakfast. That’s when your gut is most active thanks to the gastrocolic reflex. Don’t rush. Don’t strain. Just sit. Use a footstool to raise your feet so your knees are higher than your hips. This 35-degree angle mimics squatting and reduces straining by 60%.
- Move your body. Even a 20-minute walk after meals helps stimulate bowel movement. Sedentary lifestyles are a major contributor.
- Try biofeedback. If you’re straining, feeling incomplete, or have pelvic floor dysfunction, this therapy works. You’ll work with a therapist for 6 to 8 sessions, using sensors to learn how to relax the right muscles. Success rates are 70 to 80%.
When to Worry: Red Flags
Not all constipation is harmless. If you have any of these, see a doctor right away:- Unintentional weight loss of 10 pounds or more
- Bleeding from the rectum
- Stools that are much thinner than usual
- Constipation that started suddenly after age 50
- Family history of colorectal cancer
- Constipation lasting more than 6 weeks without a clear cause

What Doesn’t Work (And Why People Keep Trying It)
Many people waste months-or years-on ineffective approaches:- Drinking coffee won’t fix constipation. It might give you a temporary nudge, but it doesn’t address the root cause.
- Enemas and suppositories are fine for occasional use, but they’re not a long-term solution. They don’t retrain your colon.
- “Laxative dependency” is often misunderstood. If you need a laxative to go regularly, it’s not because you’re addicted-it’s because your body needs help moving stool. The goal is to wean off gradually once your habits improve.
- Probiotics? Some strains show promise, but most over-the-counter brands don’t have enough evidence. The Microbiome Constipation Project is studying specific bacteria like Bacteroides uniformis, but we’re not there yet.
Real Success Stories
One woman, 52, had been constipated for 15 years. She tried everything: stimulants, enemas, fiber pills. Nothing stuck. Then she started: 25g of psyllium daily, 2 liters of water, morning coffee, and sitting on the toilet with her feet on a stool for 10 minutes after breakfast. Within 8 weeks, she was going regularly without any laxatives. Another man, 68, had slow transit constipation. He was on PEG 3350 for months, but still felt bloated. His doctor added daily walks and biofeedback. After six sessions, his bowel movements became predictable and pain-free. These aren’t magic fixes. They’re consistent habits.The Bottom Line
Constipation isn’t something you just live with. It’s a signal-your body is telling you something’s off. Start with the basics: more fiber, more water, better posture on the toilet, and movement. If that doesn’t help after 4 to 6 weeks, talk to your doctor. Don’t jump to stimulant laxatives. Don’t ignore warning signs. And don’t believe the myths. Real relief comes from understanding your body, not from quick fixes.Can constipation be cured without laxatives?
Yes, for many people. Up to 60% of chronic constipation cases are normal transit type, which responds well to fiber, hydration, and toilet habits alone. Biofeedback helps those with pelvic floor issues. Lifestyle changes can restore natural bowel function without needing daily laxatives-especially if started early and followed consistently.
How long does it take for fiber to work for constipation?
It usually takes 4 to 6 weeks to see full results from increasing fiber. Your gut needs time to adjust. Add fiber slowly-no more than 5 grams every 3 to 4 days-to avoid bloating and gas. You might notice small improvements in stool consistency within a week, but regular, easy bowel movements often take longer.
Is it safe to take PEG 3350 every day?
Yes. PEG 3350 is the only laxative approved for long-term daily use. It doesn’t irritate the colon, doesn’t cause dependency, and has minimal side effects. It’s safe for months or even years if needed. Doctors recommend it as first-line treatment for chronic constipation because it works and it’s gentle.
Why do I still feel constipated even though I eat healthy?
Eating healthy doesn’t automatically mean you’re getting enough fiber or water. Many “healthy” diets (like low-carb or keto) are low in fiber. Also, constipation can be caused by medications, thyroid issues, diabetes, or pelvic floor dysfunction-not just diet. If you’re eating well and still struggling, it’s time to look beyond food.
Can stress cause constipation?
Absolutely. Stress affects the gut-brain connection. It can slow down colon motility and make pelvic floor muscles tense up, leading to straining and incomplete evacuation. People with anxiety or depression are more likely to have chronic constipation. Managing stress through movement, breathing, or therapy can improve bowel function as much as dietary changes.
When should I see a specialist for constipation?
See a gastroenterologist if you’ve tried lifestyle changes and osmotic laxatives for 8 to 12 weeks with no improvement. Also, if you have alarm symptoms like weight loss, bleeding, or sudden changes after age 50. Specialists can order tests like colonic transit studies or anorectal manometry to find the exact cause-something primary care doctors rarely do.
Do enemas help with chronic constipation?
Enemas can clear out impacted stool in emergencies, but they don’t fix the underlying issue. Using them regularly can weaken your natural bowel reflexes and make you reliant on them. They’re not a long-term solution. Focus on retraining your colon with fiber, water, posture, and movement instead.
Can constipation lead to other health problems?
Yes. Long-term straining can cause hemorrhoids, anal fissures, or rectal prolapse. Chronic constipation is also linked to increased risk of diverticulosis and may worsen symptoms in people with IBS or pelvic pain syndromes. In rare cases, stool impaction can lead to bowel obstruction or perforation. It’s not just uncomfortable-it can be dangerous if ignored.
