Calcium Supplements and Bisphosphonates: How to Avoid Absorption Problems

Dec, 22 2025
Bisphosphonate-Calcium Timing Calculator
How to Use This Calculator
Enter your bisphosphonate dose time and type to see when you can safely take calcium supplements and other medications.
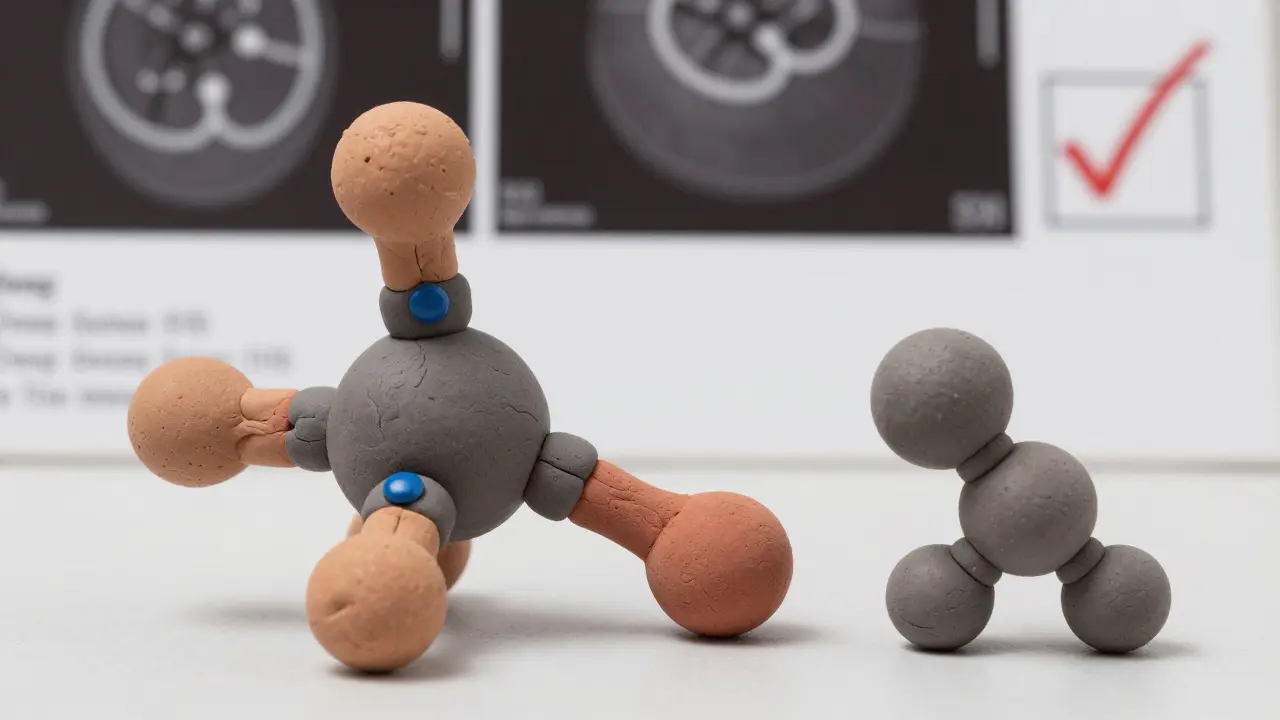
When you’re taking bisphosphonates for osteoporosis, the goal is simple: strengthen your bones and prevent fractures. But if you’re also taking calcium supplements - and most people are - you might be accidentally sabotaging your treatment. The problem isn’t that calcium is bad. It’s that calcium supplements and bisphosphonates don’t play well together. When taken too close, they bind in your gut and form a compound your body can’t absorb. That means your bisphosphonate, which costs money and requires strict dosing, becomes nearly useless.
Why Calcium Ruins Bisphosphonate Absorption
Bisphosphonates like alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) are designed to slow bone loss. They work by sticking to bone surfaces and blocking cells that break down bone tissue. But here’s the catch: these drugs are poorly absorbed to begin with. Only about 1% of the pill you swallow actually makes it into your bloodstream. That’s why timing matters so much. Calcium - whether from a supplement or dairy - grabs onto bisphosphonates in your stomach and intestines. Think of it like magnets sticking together. The two molecules lock up, forming an insoluble clump that just passes through your body. Studies show that taking calcium carbonate with alendronate cuts absorption by 94%. Calcium citrate isn’t much better - it still reduces absorption by 88%. That’s not a small drop. That’s treatment failure.The Exact Timing Rules You Need to Follow
There’s no wiggle room here. If you want your bisphosphonate to work, you must follow the rules exactly:- Take your bisphosphonate first thing in the morning, on an empty stomach.
- Use only plain water - no coffee, tea, juice, milk, or soda.
- Wait 30 to 60 minutes before eating, drinking anything else, or taking other medications.
- Stay upright - sitting or standing - for the full waiting period. Lying down increases your risk of esophageal irritation by 62%.
When to Take Calcium Supplements (And Vitamin D)
Calcium isn’t the enemy - it’s essential. But you need to separate it from your bisphosphonate. The safest window is at least two hours after your bisphosphonate dose. That means if you take your pill at 7 a.m., don’t touch calcium until after 9 a.m. The best time to take calcium supplements is with dinner. Why? Because your body absorbs calcium better with food, and dinner is usually the last thing you eat before bed. This also gives you a full 12+ hours between your bisphosphonate and calcium. Vitamin D, which helps calcium get into your bones, should also be taken with your evening meal. No need to time it with your bisphosphonate - vitamin D doesn’t interfere.
What About IV Bisphosphonates?
If the morning ritual feels impossible, you’re not alone. Many patients - especially older adults with multiple medications - switch to intravenous (IV) bisphosphonates like zoledronic acid (Reclast). These are given once a year in a doctor’s office. No fasting. No waiting. No risk of calcium interference. But there’s a trade-off. IV bisphosphonates can cause flu-like symptoms after the first infusion - fever, muscle aches, fatigue - in 15% to 30% of people. These usually go away in 24 to 48 hours. Your doctor will check your calcium and vitamin D levels before the infusion. If they’re too low, you’ll need to fix that first. Otherwise, you risk dangerous drops in blood calcium after the shot.Why So Many People Fail - And How to Succeed
Here’s the hard truth: only about 42% of patients follow the timing rules correctly after six months. Why? Because it’s hard. Coffee in the morning? Check. Breakfast with toast and yogurt? Check. Pills for blood pressure, thyroid, or cholesterol? All stacked on the counter. It’s easy to forget - or assume it doesn’t matter. A 2022 Johns Hopkins study followed a 79-year-old woman who took her bisphosphonate with her morning calcium pill. She thought she was doing everything right. She didn’t realize the two were canceling each other out. Within 18 months, she had two broken vertebrae. Her bisphosphonate was useless. The fix? Simple systems.- Use a pill organizer with labeled compartments: “Bisphosphonate AM” and “Calcium PM.”
- Set two phone alarms: one for 7 a.m. (take bisphosphonate), one for 7 p.m. (take calcium).
- Download the National Osteoporosis Foundation’s free app. It sends reminders with exact timing instructions - and 65% of users who used it improved adherence.
What Your Doctor Should Check Before You Start
Before you even take your first bisphosphonate, your doctor should test your blood for:- 25-hydroxyvitamin D - should be above 30 ng/mL
- Serum calcium - should be above 8.5 mg/dL
- Parathyroid hormone (PTH) - to rule out overactive glands
- Phosphorus - to ensure balance
What to Do If You Mess Up
If you accidentally take calcium with your bisphosphonate, don’t panic. Don’t double-dose. Don’t try to make up for it. Just skip that day’s bisphosphonate. Wait until tomorrow morning. Start fresh. Take it with plain water on an empty stomach. Resume your normal schedule. Taking two doses close together won’t help - it’ll just increase your risk of stomach upset or esophageal damage. The goal isn’t perfection. It’s consistency over time.Alternatives If the Timing Is Too Hard
If you’ve tried and failed to stick to the rules, you’re not alone. And you’re not out of options. Denosumab (Prolia) is a monthly injection that doesn’t require fasting or upright waiting. It’s effective, especially for people with kidney issues. But it’s more expensive and requires strict adherence to injection timing. Abaloparatide (Tymlos) is a daily injection that builds bone instead of just slowing loss. It doesn’t interact with calcium. But it costs over $2,900 a month - far more than generic bisphosphonates. Your doctor might suggest switching if you’ve had two failed attempts at oral bisphosphonates. But don’t quit without talking to them. Many people who thought they couldn’t manage the timing ended up succeeding with simple tools and support.Bottom Line: Timing Is Everything
Calcium supplements and bisphosphonates can work together - but only if you keep them apart. The difference between success and failure isn’t genetics. It’s not luck. It’s a 30-minute window. It’s a glass of plain water. It’s staying upright. It’s waiting. If you’re taking both, write down your schedule. Set alarms. Use a pill box. Talk to your pharmacist. Ask your doctor to review your routine. Millions of people take these drugs. Most of them fail because they don’t know how to time them right. You don’t have to be one of them.Can I take calcium and bisphosphonates at the same time?
No. Taking calcium supplements at the same time as bisphosphonates reduces the absorption of the bisphosphonate by up to 94%. Always separate them by at least two hours. Take your bisphosphonate first thing in the morning on an empty stomach, and take calcium with dinner.
What if I forget and take them together?
Skip your bisphosphonate for that day. Don’t take a double dose tomorrow. Just restart your regular schedule the next morning with plain water and an empty stomach. Missing one dose won’t ruin your treatment - but continuing to mix them will.
Can I drink coffee or tea with my bisphosphonate?
No. Coffee, tea, juice, and even mineral water can reduce bisphosphonate absorption by 50% to 60%. Only plain water is safe. Wait at least 30 to 60 minutes after taking your pill before drinking anything else.
Do I need to stay upright for the full 30-60 minutes?
Yes. Lying down increases the risk of the pill getting stuck in your esophagus, which can cause irritation, ulcers, or even bleeding. Stay sitting or standing for the full waiting period. Set a timer if you need to.
Is there an easier way to take bisphosphonates?
Yes. Intravenous bisphosphonates like zoledronic acid are given once a year by injection and don’t require fasting or upright waiting. But they can cause flu-like symptoms after the first dose. Talk to your doctor if the daily routine is too hard to manage.
How do I know if my bisphosphonate is working?
Bone density scans (DEXA) are the best way to track progress. Most people see improvement after one year, especially if they’ve followed timing rules. Your doctor should schedule a scan every one to two years. If your bone density drops or stays the same, your absorption may be poor - and timing could be the issue.
Should I take vitamin D with calcium?
Yes. Vitamin D helps your body absorb calcium and supports bone health. Take it with your evening meal, along with your calcium supplement. It doesn’t interfere with bisphosphonates, so timing isn’t an issue.
What if I have GERD or trouble staying upright?
If you have GERD, esophageal strictures, or can’t sit up for 30-60 minutes, oral bisphosphonates may not be safe. Talk to your doctor about alternatives like denosumab (Prolia) or IV bisphosphonates. For some, the risks of esophageal damage outweigh the benefits of oral treatment.
