Medication Safety and Mental Health: How to Coordinate Care to Prevent Harm

Nov, 24 2025
When someone is managing a mental health condition like depression, bipolar disorder, or schizophrenia, medication isn’t just part of treatment-it’s often the difference between stability and crisis. But here’s the problem: medication safety in mental health is one of the most overlooked areas in healthcare. People are getting the right drugs, but they’re not always getting them safely. Doses are missed. Medications are stopped abruptly. Drugs interact in dangerous ways. And too often, no one is checking if it’s even working.
Think about this: lithium, a common mood stabilizer, can be life-saving. But if blood levels aren’t monitored every three months, it can turn toxic. Clozapine, used for treatment-resistant schizophrenia, requires weekly blood tests to catch a rare but deadly drop in white blood cells. Yet in England, only 40% of patients on lithium get those essential checks. That’s not a glitch. That’s a system failure.
Why Mental Health Medications Are Different
Psychotropic medications don’t work like antibiotics or blood pressure pills. They affect the brain. And the brain doesn’t always tell you when something’s wrong. A person on antipsychotics might feel sluggish or dizzy but not report it, thinking it’s just part of their condition. Someone on antidepressants might stop taking them because they feel better-only to crash weeks later when withdrawal hits.
There are also hidden risks. People with serious mental illness are more likely to be prescribed multiple medications at once-antidepressants, antipsychotics, sleep aids, painkillers, even drugs for substance use. This is called polypharmacy. It’s not always necessary. Sometimes it’s accidental. And it’s dangerous. Mixing certain drugs can cause seizures, heart rhythm problems, or extreme sedation. One wrong combination can land someone in the hospital-or worse.
Then there’s the human side. Mental health conditions can make communication harder. Cognitive fog, paranoia, or lack of insight mean patients may not understand why they’re taking a pill-or may refuse it. Some may hoard meds for later use. Others might sell them. Medication diversion is real. In prisons, where mental illness rates are 3 to 5 times higher than the general population, it’s a major issue. Community care isn’t immune.
The Three Big Problems
Medication errors in mental health don’t happen by accident. They’re the result of three overlapping failures:
- Medications themselves-Some psychotropics are high-alert drugs. That means even small mistakes can cause serious harm. Lithium, clozapine, benzodiazepines, and certain antipsychotics are on that list.
- Provider and patient factors-Clinicians may not know the full mental health history. Patients may not tell them about over-the-counter meds, herbal supplements, or street drugs. Communication breaks down between GPs, psychiatrists, pharmacists, and case workers.
- System failures-Paper records get lost. Prescriptions are handwritten and illegible. Transitions between hospital, community care, and prison happen without proper handovers. No one checks if meds are still needed.
These aren’t theoretical risks. They’re happening every day. A 2021 review from New Zealand’s Health Quality & Safety Commission found that over half of mental health patients had at least one medication discrepancy during a care transition. That’s not a typo. Half.
What Works: The Proven Fixes
There are solutions. They’re not fancy. They’re simple. And they work-if they’re used consistently.
Medicines reconciliation is the cornerstone. It’s not just asking, “What meds are you on?” It’s verifying every single one-prescribed, bought over the counter, or taken without a prescription. You compare what the patient says, what the pharmacy says, what the hospital says, and what the GP says. Then you fix the gaps. Done right, this cuts medication errors by up to 70%.
Electronic prescribing is another game-changer. Digital systems stop illegible handwriting, prevent duplicate prescriptions, and flag dangerous interactions. In New Zealand, hospitals that switched to e-prescribing saw a 55% drop in prescribing errors. In Australia, the Medication Safety Standard (updated in 2022) now requires all community mental health services to use digital tools where possible.
Clinical pharmacists are critical. They’re not just the people who hand out pills. They’re the ones who spot the double-dosing, the drug interactions, the unnecessary meds. A pharmacist embedded in a mental health team can reduce errors by 25%. Yet in many places, they’re still seen as optional.
The ten rights and three checks aren’t just for nurses. They’re for everyone involved. Right patient. Right medication. Right dose. Right route. Right time. Right documentation. Right reason. Right response. Right to refuse. Right education. And three checks: when you pull it, when you prepare it, when you give it. It sounds basic. But in a rushed clinic or a chaotic ward, skipping one check can cost someone their life.

Special Cases: Lithium, Clozapine, and High-Risk Drugs
Some medications need extra layers of safety.
Lithium requires monthly blood tests for the first three months, then every three months after that. The therapeutic range is narrow. Too low? It doesn’t work. Too high? It causes tremors, confusion, kidney damage, or cardiac arrest. NICE guidelines say this clearly. But in real life? Many GPs don’t know the schedule. Patients forget. Labs don’t flag it. That’s why some clinics now use automated alerts in electronic records-when a lithium test is due, the system pings the clinician and the patient.
Clozapine is even stricter. Blood counts must be checked weekly for the first 18 weeks, then every two weeks, then monthly. If the white cell count drops below a certain level, the drug must stop immediately. In Australia, the Clozapine Registry tracks every patient on the drug. If a test is missed, the system flags it. That’s how it should be done.
And then there’s the off-label use of antidepressants-like mirtazapine-for sleep or sedation. It’s common. But it’s risky. These drugs can be diverted. They can cause weight gain, dizziness, and dependence. NHS England specifically warns against this practice. Yet it still happens. Why? Because it’s easier than prescribing a real sleep aid or doing behavioral therapy.
Coordination Is Everything
The biggest danger isn’t the drug. It’s the gap between services.
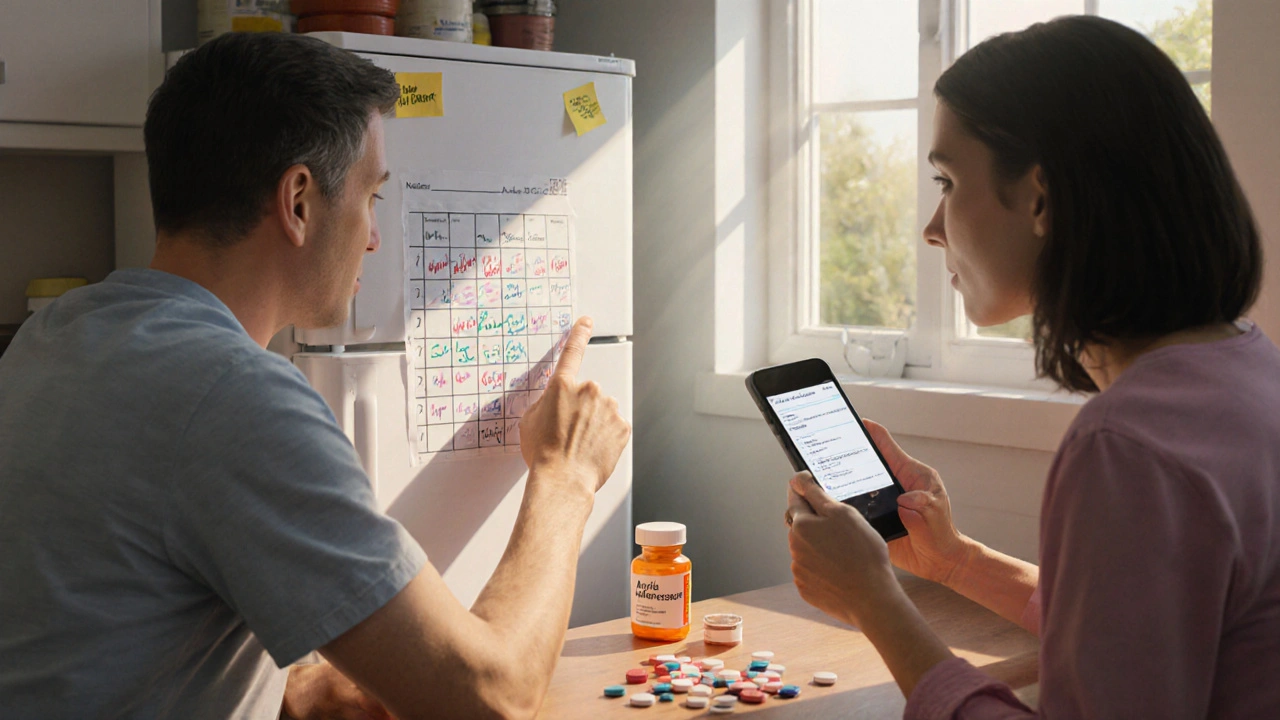
Imagine someone discharged from a psychiatric hospital. They’re on five medications. The hospital sends a summary to their GP. But the GP hasn’t seen the patient in two years. The pharmacy doesn’t know about the new meds. The case worker doesn’t know the dosage schedule. Three weeks later, the patient stops taking one drug because they felt fine. Then they get worse. No one connects the dots.
That’s why coordinated care isn’t optional. It’s essential. Successful models include:
- Joint case conferences between GPs and psychiatrists
- Medicines management coordinators-often pharmacists-who track all meds across settings
- Shared digital records that update in real time
- Clear written care plans that list every medication, its purpose, monitoring needs, and who to call if symptoms worsen
NHS England’s guidance says every mental health medicine must have a documented reason. Not just “for depression.” But “for depressive episode with anxiety, started 03/2025, target dose 20mg, monitor for weight gain and sedation.” That’s specificity. That’s safety.
What Patients and Families Can Do
You don’t have to wait for the system to fix itself. Here’s what you can do:
- Keep a written list of every medication-name, dose, why you take it, and when. Include vitamins, supplements, and herbal remedies.
- Ask: “Is this still needed?” “What happens if I stop it?” “Are there side effects I should watch for?”
- Bring your list to every appointment-GP, psychiatrist, pharmacist, ER.
- If you’re switching providers, ask for a copy of your medication record before you leave.
- Don’t stop meds suddenly, even if you feel better. Some cause withdrawal seizures or rebound symptoms.
And if you’re a caregiver: speak up. If you notice someone is confused, drowsy, or acting differently after a med change, don’t assume it’s their illness. Ask: “Did their meds change?”
The Bottom Line
Medication safety in mental health isn’t about being perfect. It’s about being consistent. It’s about checking. Confirming. Documenting. Coordinating. It’s about treating psychotropic drugs like the powerful, risky tools they are-not like candy.
Every person on mental health meds deserves a care plan that’s clear, updated, and shared. They deserve to know why each pill is in their hand. They deserve blood tests when needed. They deserve a pharmacist who checks for interactions. They deserve a system that doesn’t let them fall through the cracks.
It’s not complicated. But it does require effort. From clinicians. From pharmacists. From patients. From families. From policymakers.
Because when medication safety fails in mental health, the cost isn’t just medical. It’s human.
Why are psychotropic medications more dangerous than other drugs?
Psychotropic drugs affect brain chemistry, which can make side effects harder to detect and more dangerous. They often require strict monitoring-like blood tests for lithium or clozapine-and have narrow safety margins. Even small mistakes in dose or timing can lead to seizures, organ damage, or death. Plus, mental health conditions can impair a person’s ability to report symptoms or follow instructions, increasing the risk of harm.
What is medicines reconciliation, and why is it important?
Medicines reconciliation is the process of comparing a patient’s current medication list with what’s been prescribed or administered during a care transition-like moving from hospital to home or between clinics. It catches errors like missing drugs, wrong doses, or duplicates. Studies show it reduces medication errors by up to 70%. Without it, patients often get the wrong meds or stop taking needed ones, leading to relapse or hospital readmission.
Can I stop my mental health medication if I feel better?
No-not without talking to your doctor. Many psychotropic drugs, especially antidepressants and antipsychotics, can cause withdrawal symptoms if stopped suddenly. These include anxiety, insomnia, nausea, dizziness, or even seizures. Even if you feel fine, your brain may still need the medication to stay balanced. Always taper off slowly under medical supervision.
How often should I get blood tests if I’m on lithium or clozapine?
For lithium, blood levels should be checked every three months after the first few months of treatment. For clozapine, weekly blood tests are required for the first 18 weeks, then every two weeks, then monthly. These tests are non-negotiable-they catch life-threatening drops in white blood cells (clozapine) or toxic lithium levels. If your doctor doesn’t schedule these, ask for them.
What should I do if I think my meds are causing side effects?
Write down the symptoms-when they started, how bad they are, and what you were taking at the time. Bring this to your next appointment. Don’t assume it’s just your illness. Many side effects-like weight gain, tremors, or confusion-are medication-related. Ask your doctor or pharmacist: “Could this be from my meds?” and “Is there a safer alternative?”
Are electronic prescribing systems really better than paper?
Yes. Studies show electronic systems reduce prescribing errors by 30-55%. They prevent illegible handwriting, flag dangerous drug interactions, and alert clinicians to duplicate prescriptions or missed monitoring. Paper systems rely on memory and manual checks-which is why errors are so common in mental health care.
If you’re on mental health medication, your safety doesn’t depend on luck. It depends on clarity, communication, and consistent checks. Don’t wait for someone else to fix the system. Be the person who asks the questions. Keep the list. Show up. Speak up. Your life depends on it.
